Regional Anaesthesia
Tutorial 53
Questions
- In relation to ANAL BLOCKS:
- For which procedures is this block indicated?
- Describe the areas you would infiltrate.
- How much local anaesthetic would you inject at each site?
- INGUINAL HERNIA FIELD:
- Name the nerves which supply the inguinal hernia field.
- Which landmarks would you use to block these nerves?
- The 2 ‘pop’ sensations are caused by which anatomical structures?
- The PENILE BLOCK in adults:
- What type of drug should never be used when performing a penile block in adults?
- Describe how you would reach the target site below the pubis symphysis.
- What structure makes it important to aspirate prior to injection?
- The PENILE BLOCK in children:
- What type of drug should never be used when performing a penile block in children?
- When performing a ring block, what should you be cautious about?
- Should children be asleep for this block?
- PUDENDAL BLOCK:
- Describe how you would perform a pudendal block.
- Why would this block not be suitable for cavity and rotational forceps?
- What possible maternal complications could arise?
THE ANAL BLOCK
INTRODUCTION
- The anal block is also known as the perianal block and the posterior perineal block.
- The aim is to block the inferior rectal nerve which is a branch of the pudendal nerve.
- This is an ideal field block for haemorrhoidectomy as it is invariably successful – even in inexperienced hands.
- Although it provides good anaesthesia for rectal operations, it is usually combined with general anaesthesia or heavy sedation. Patients find surgery of this nature embarrassing and most would prefer to be oblivious to their surroundings.
- There is no risk of urinary retention.
INDICATIONS
- Haemorrhoidectomy.
- Anal dilation / stretching.
- Anal fissure surgery.
EQUIPMENT
- 20 ml plastic syringe.
- 22 G (38mm) needle – sharp.
- Gloves and antiseptic paint.
TECHNIQUE
- Sedation or general anaesthesia.
- Lithotomy position.
- Paint and drape patient.
- Inject a subcutaneous circle of local anaesthesia around the anus (radius of 2.5 cm).
- Use approximately 10 ml of local anaesthetic.
- Imagine you are looking at a clock face. Take the 22 G (38mm) needle and insert it at the 3 o’clock position on the above circle.
- Insert the needle to the hilt (angle it at 45° laterally) and inject 3 – 4 ml as the needle is withdrawn.
- Reinsert at 12 o’clock (angled 45° north) and inject 3 – 4 ml on withdrawal and again at 6 o’clock (angled 45° south) injecting 3 – 4 ml on withdrawal.
- Insert the needle at 9 o’clock and repeat the same sequence.
- The total amount of local anaesthetic used in this block is in the order of 30 – 35 ml.
- It is good practice to insert a gloved index finger into the rectum whilst injecting to ensure the rectal mucosa is not perforated.
DRUGS
- Bupivacaine and ropivacaine work almost as quickly as lidocaine so use the longer acting agents to obtain the benefit of prolonged post operative analgesia.
- Bupivacaine 0.25% or ropivacaine 0.4%. It is reasonable to add epinephrine 1:200,000.
- This block should give good analgesia lasting 4-8 hours.
IMPORTANT POINTS
- If the needle perforates the rectal mucosa there is a risk of an ischiorectal abscess developing.
- Buttock haematomas can occur but are not usually a significant problem.
- This is a better block than a saddle block or caudal for haemorrhoidal surgery as it doesn’t affect the legs and does not cause urinary retention.
- It is a simple and reliable block. I believe it should be performed for all superficial anal surgery.
INGUINAL HERNIA FIELD BLOCK
INTRODUCTION
- The inguinal field block is used in conjunction with general anaesthesia for surgical repair of an inguinal hernia.
- In high risk patients it may be used as a sole anaesthetic technique. When used it this way the anaesthetic block is not altogether satisfactory and the surgeon usually has to infiltrate LA throughout the operation.
- This block gives excellent post operative analgesia of 8 – 12 hours duration.
ANATOMY
- The operative area is supplied by the iliohypogastric, ilioinguinal and genitofemoral nerves along with branches from bilateral intercostal nerves.
- The iliohypogastric nerve (L1) supplies the skin above the inguinal ligament. It overlaps with its corresponding nerve at the centre line suprapubically.
- The ilioinguinal nerve (L1) runs parallel to and below the iliohypogastric nerve. It supplies the scrotal skin (labia) and upper thigh.
- The genitofemoral nerve (L1 and L2) has two components. The genital accompanies the spermatic cord and supplies the scrotal skin (labia). The femoral branch supplies the skin over the femoral triangle.
- The intercostal nerves run subcutaneously, obliquely down over the lower abdomen. They crossover with their opposite nerves at the midline.
- Thus, three nerves must be blocked together with the spray of subcutaneous intercostal nerves.
INDICATIONS
- Many surgeons use this block routinely as an adjunct to general anaesthesia and to provide post operative pain relief.
- High risk elderly men presenting acutely with a strangulated hernia. A spinal or GA may be more suitable but it is possible to perform such surgery with this block as the sole anaesthetic.
EQUIPMENT
- Plastic 20 ml syringe.
- Insulin syringe and fine needle for subcutaneous infiltration.
- Marker pen.
- 22 G short bevel 50 mm needle.
- 22 G spinal needle 90 mm.
- 18 G needle – to make an oversize hole in the skin for the 22 G short bevel needle to slide easily.
- Gloves, drapes and prep solution.
- Monitoring (SpO2, ECG, BP).
- Resuscitation equipment.
TECHNIQUE
- Take the marker pen and draw a line from the anterior superior iliac spine (ASIS) to the umbilicus. [Fig 18]
- From the ASIS, travel 2.5 cm along this line and inject a subcutaneous bleb of LA. At this point, make a hole in the skin with the 18 G needle. This allows the 22 G needle to slide freely and thus makes it easier to elicit loss of resistance.
- Insert the 22 G 50 mm short bevel needle at right angles to the skin. At a depth of 2 cm (depends on adipose tissue depth) the needle will hit the external oblique muscle aponeurosis. “Trampoline” the needle gently up and down, gradually increasing the downward pressure with each bounce until you feel it ‘pop’ through. The needle tip now lies between the external and internal oblique layers. The iliohypogastric nerve runs here and 10 ml of LA is injected.
- Advance another few millimetres and a second ‘pop’ is experienced as the needle tip perforates internal oblique. The ilioinguinal nerve runs here and 10 ml of LA is injected.
- Find the midpoint of the inguinal ligament and mark a spot 1 cm above the midpoint. Infiltrate a subcutaneous bleb of LA and make a hole with the large 18 g needle. Insert the 22 G short bevel needle vertically. At 2 cm a ‘pop’ is felt and a second ‘pop’ at approximately 4 cm. Inject 20 ml of LA to block the genitofemoral nerve. (It may be preferable to ask the surgeon to infiltrate this nerve under direct vision during the surgery).
- To block the intercostal nerves, infiltrate along the line of the proposed incision using the 90 mm spinal needle. Make sure you infiltrate 2 – 3 cm above and below the incision. Approximately 20 ml should suffice.
- Finally, inject a few ml of LA subcutaneously around the pubic tubercle.
- Note that approximately 50 – 60 mls of LA is used altogether.
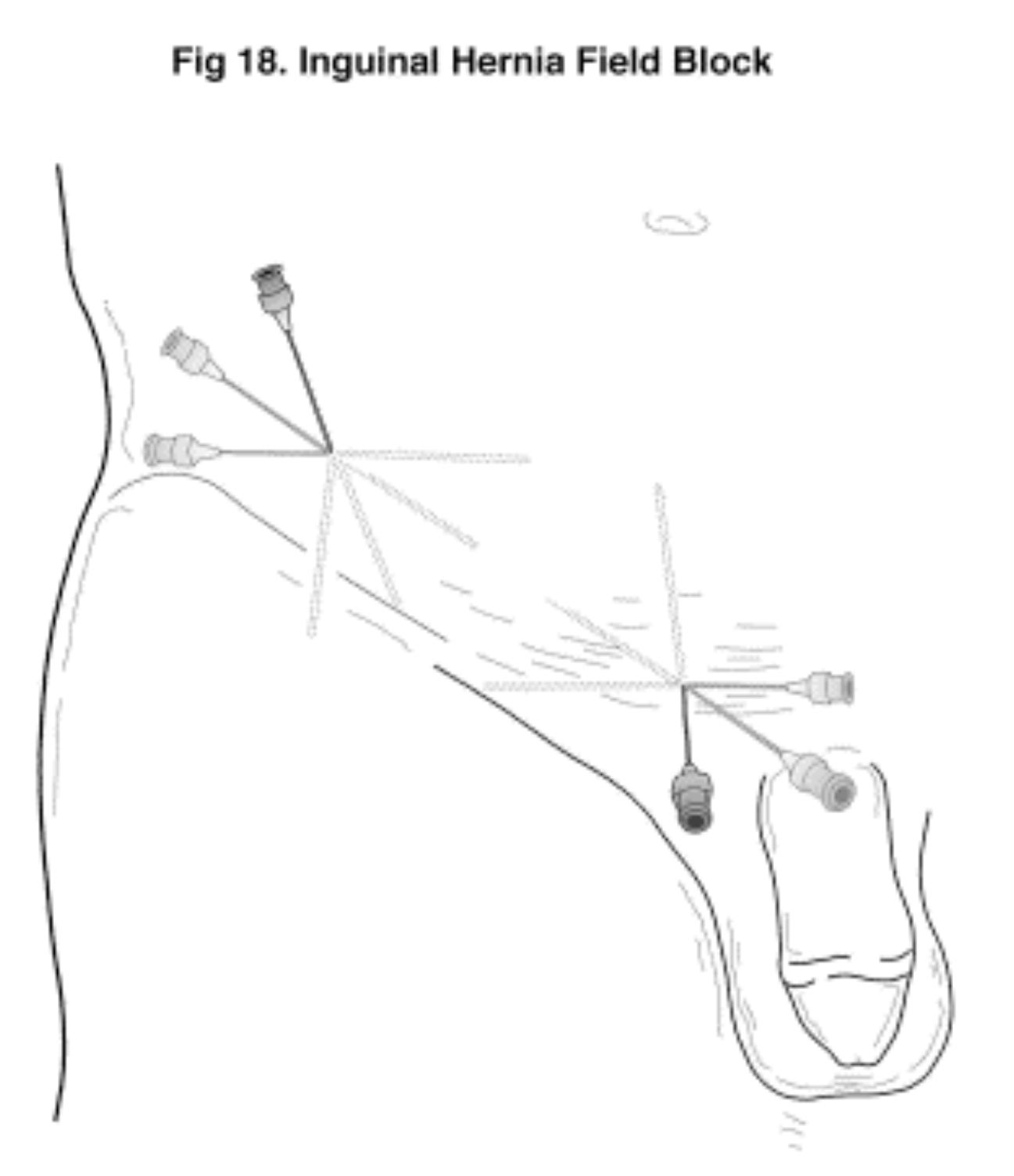
Figure 18 (Click to enlarge)
DRUGS
- Use bupivacaine or ropivacaine as the prolonged post operative analgesia is usually an advantage.
- The maximum safe dose of bupivacaine is 2 mg / kg (and 3 – 4 mg / kg of ropivacaine).
- 50 – 60 ml of LA is required. An 80 kg man could be given 160 mg of bupivacaine. Draw up 32 ml of bupivacaine 0.5% and dilute it with 28 ml of saline to give 60 ml.
- Clonidine 1 – 2 mcg / kg could be added to prolong and intensify the block.
- Epinephrine 1:200,000 will give an added safety margin but will not greatly prolong the block.
IMPORTANT POINTS
- This is not an easy block in very obese patients as the landmarks are obscured.
- The femoral nerve may be blocked by a ‘spillover’ effect.
- In children the block may be simplified. The child should be anaesthetised (ie GA). Insert the 22 G shallow bevel needle at a point 1 cm medial to the ASIS and when the first ‘pop’ is felt inject 0.75 ml / kg of LA. Then fan a few ml subcutaneously along the proposed incision line.
- In infants the surgeon should infiltrate as he goes. Be VERY careful with the maximum safe dose (eg 6 mg of bupivacaine in a 3 kg neonate).
- In the paediatric population this block is suitable for herniotomy, hydrocoele and orchidopexy.
- Be careful with this block. It requires using a large volume of LA in a very vascular region and the risk of toxicity is real.
PENILE BLOCK
INTRODUCTION
- The penile block is commonly used in conjunction with general anaesthesia for surgical procedures on the penis (eg circumcision, hypospadias repair). If a long acting local anaesthetic agent is used, post operative analgesia of 8 – 12 hours duration can be expected.
- In infants and small children, all that is required is a small volume of subcutaneous LA at the root of the penis. In these cases a ringblock is satisfactory.
- The technique outlined here is easy to perform and has a high success rate.
- NEVER use vasoconstrictors in the LA solution. The penile arteries are end arteries and vasoconstriction of these vessels risks penile ischaemia or worse.
ANATOMY [Fig 19] and [Fig 20]
- The shaft of the penis contains three tube like structures.
- Two parallel tubes (the corpora cavernosa) run along the dorsal aspect and a single tube (the corpus spongiosum) runs anteriorly. The urethra is contained within the corpus spongiosum.
- All three tubes are wrapped in a tough fascia (Bucks fascia).
- The penis is slung from the overlying superficial fascia by the suspensory ligament. This ligament splits and fuses with Bucks fascia.
- The dorsal nerves accompany the artery and veins. All are enclosed in the space provided by the split suspensory ligament.
- The two parallel dorsal nerves supply most of the penis. They are branches of the pudendal nerves.
- The base and proximo-ventral aspect of the penis is supplied by branches of the genitofemoral and ilioinguinal nerves.
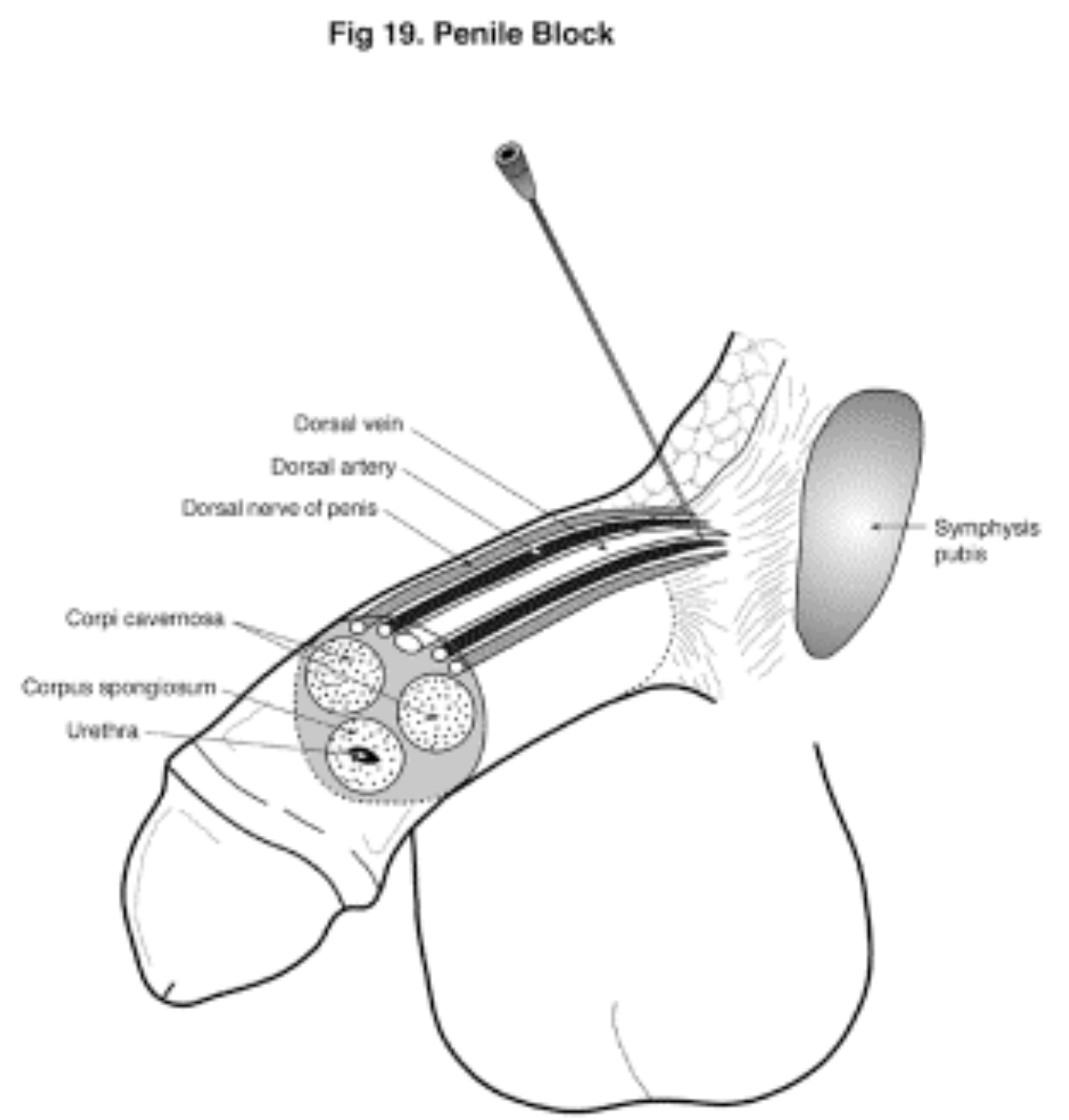
Figure 19 (Click to enlarge)
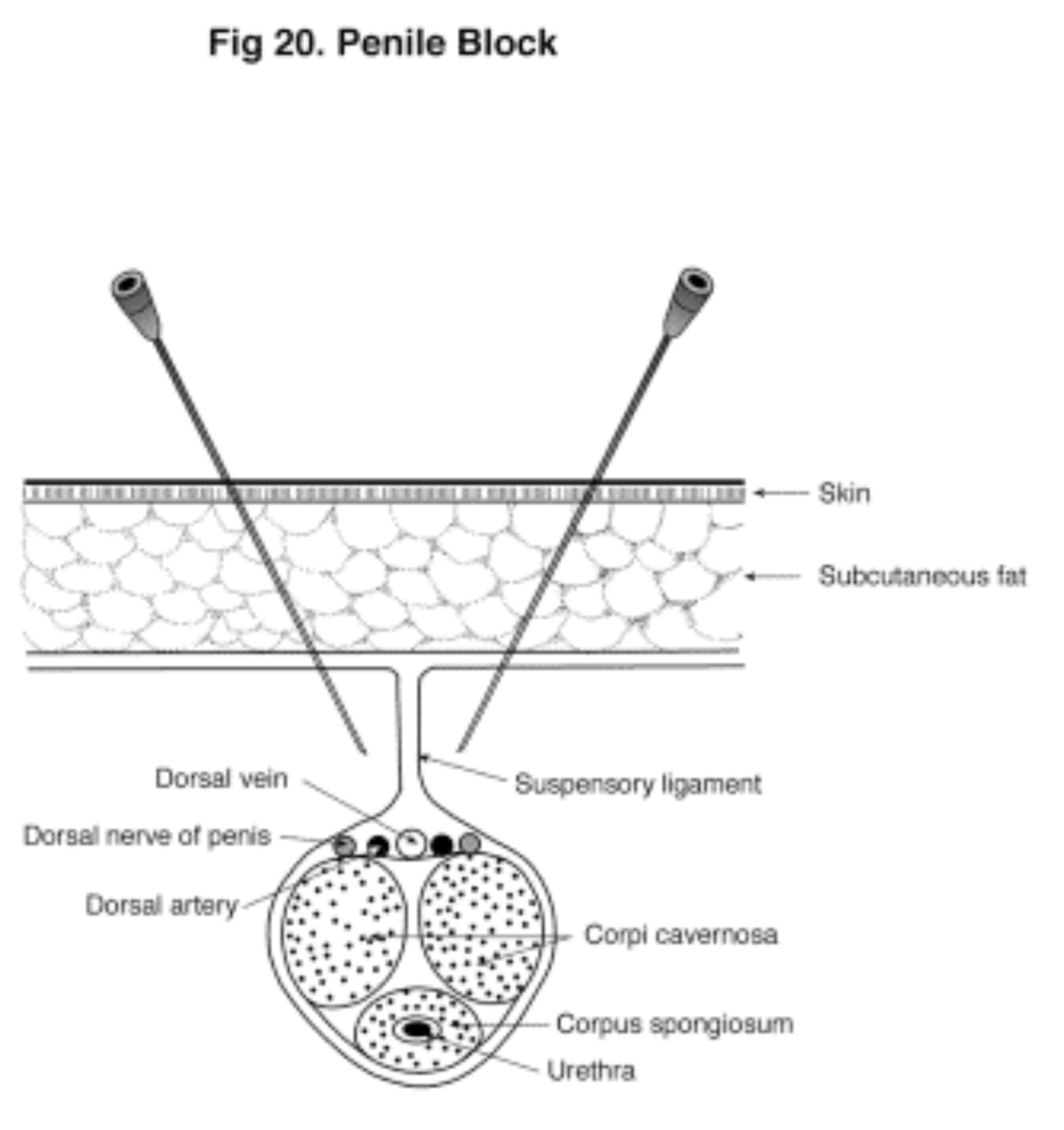
Figure 20 (Click to enlarge)
INDICATIONS
- Circumcision, hypospadias repair, meatoplasty and penile trauma surgery.
EQUIPMENT
- Insulin syringe and fine needle for subcutaneous infiltration.
- ADULTS: 22 G 50 mm short bevel needle with fine bore plastic tubing attached + 20 ml plastic syringe.
- CHILDREN: 25 G 25mm needle + 5 or 10 ml plastic syringe.
- Gloves, drapes and antiseptic solution.
TECHNIQUE
ADULTS:
- Paint with povidone / iodine solution.
- Infiltrate blebs of subcutaneous LA (insulin syringe) if patient is awake.
- Place your index finger on the underside of the symphysis pubis at the root of the penis.
- The intention is to place LA on each side of the suspensory ligament. The LA will then diffuse across the fascia and into the “neurovascular bundle”.
- Insert a 22 G 50 mm short bevel needle at 10.30 o’clock at the root of the penis. Advance it until it contacts the bony symphysis. Note the depth. [Fig 20]
- Withdraw and reinsert to pass beneath the symphysis. At a depth of 2 – 3 cm you will feel the resistant superficial fascia. ‘Pop’ through this. The needle tip has now reached its target.
- Check aspiration and inject 10 ml of local anaesthetic.
- Repeat this procedure at 1.30 o’clock.
- The terminal branches of the ilioinguinal and genitofemoral nerves are blocked by infiltrating a subcutaneous line of LA (3 – 5ml approx) on the ventral aspect where the shaft meets the scrotum.
- The advantage of this technique is that the needle is directed away from the neurovascular bundle. The LA is deposited on either side of the suspensory ligament and diffuses across the fascia to block the nerves.
CHILDREN:
- Children should be asleep for this block.
- In children the dorsal nerves are virtually subcutaneous and it is unnecessary to use the adult technique.
- Paint with povidone / iodine solution.
- Take a 5 ml syringe of LA and a 25 G 25 mm needle.
- At the root of the penis (dorsal aspect) inject a subcutaneous infiltration of LA from 10 o’clock to 2 o’clock.
- Inject a line of subcutaneous LA approximately 1 cm long on the ventral surface at the junction of the shaft and scrotum.
- Many anaesthetists simply perform a complete subcutaneous ring block at the root of the penis. This is quite satisfactory.
- The advantage of this technique is that the needle is kept away from the dorsal vessels and the corpora cavernosa. This reduces the risk of haematoma.
DRUGS
ADULTS:
- NEVER USE A VASOCONSTRICTOR
- 10 ml of bupivacaine 0.25% at 10.30 and 1.30 o’clock plus 3-5 ml at the penile-scrotal junction. (or ropivacaine 0.4%).
- The onset of the block is more rapid if a mixture of lidocaine /bupivacaine is used (ie 1/3 lidocaine 1% + 2/3 bupivacaine 0.25%).
CHILDREN:
- NEVER USE A VASOCONSTRICTOR
- Use 0.25% bupivacaine plain (or 0.4% ropivacaine plain) 3.
- Dose varies from 2 ml in an infant to 7 ml in a 10 year old.
- The expected duration of analgesia is 6 – 8 hours.
IMPORTANT POINTS
- Repeat: don’t use vasoconstrictors.
- Haematomas can form and compress vessels leading to ischaemia.
- When using the subcutaneous ring block technique, be careful not to inject so much LA that a tourniquet effect is caused. This causes venous oozing which makes surgery difficult.
THE PUDENDAL BLOCK
INTRODUCTION
- In the past 20 – 30 years, epidural anaesthesia and subarachnoid blockade have largely superseded the traditional obstetric anaesthetic techniques (caudal, paracervical and pudendal blocks).
- However there is still a place for these blocks and many obstetricians value the fact that they are simple, quick and reasonably reliable.
- In the first stage of labour, regular uterine contractions cause progressive dilation of the cervix. When the cervix is fully dilated (approx. 10 cm), the first stage is over and the second stage begins.
- In the second stage of labour, the foetus moves down the birth canal. The second stage ends with delivery of the baby.
- Cervical dilation can be very painful and this can be relieved with a paracervical block. This involves injecting a large volume of LA into a very vascular region immediately adjacent to the foetal head.
- There have been many recorded incidences of maternal toxicity due to the rapid LA absorption. Intrafoetal and intraplacental injections of LA have also occurred.
- The paracervical block is best left to experienced obstetricians or anaesthetists.
- The pudendal nerve (S2,3,4) supplies the lower third of the vagina and the perineum. A bilateral pudendal block eases the pain caused by the stretching of the birth canal as the foetus passes through. It also provides good anaesthesia for an episiotomy.
ANATOMY
- The pudendal nerve accompanied by it companion artery and vein passes just behind the junction of the sacrococcygeal ligament and the ischial spine.
- The needle is introduced transvaginally and through the sacrococcygeal ligament near the spine. The pudendal nerve lies on the far side of this ligament.
INDICATIONS
- Anaesthesia for the lower vagina and perineum to allow outlet forceps delivery and episiotomy.
EQUIPMENT
- 20 G (120 mm) needle.
- 20 ml plastic syringe.
- A needle guide is available for this injection (the Iowa trumpet and the Kobak needle + guide). This is not absolutely necessary but it does make the procedure easier and safer.
- Antiseptic paint for vagina (eg chlorhexidine).
- Gloves, drapes etc.
TECHNIQUE
- The ideal position is lithotomy but supine with the legs drawn up is satisfactory.
- Paint the vagina and perineum. Drape.
- To block the patients left pudendal nerve, insert your left index and middle fingers into the vagina and place the tips of these fingers on the ischial spine. [Fig 21]
- Take the syringe, needle and guide in your right hand and place the tip of the guide just below the spine. Introduce the needle via the guide and pierce the vaginal epithelium and the underlying sacrococcygeal ligament.
- Whilst the needle tip is in the sacrococcygeal ligament there is almost total resistance to injection. When the tip emerges on the far side there is a loss of resistance. The tip now lies beside the pudendal nerve.
- Perform a check aspiration and inject 10 ml of LA.
- Repeat the procedure on the other side to block the right pudendal nerve.
- Within minutes there is a good sensory block to the lower vagina and perineum. You may also need to infiltrate subcutaneously along the lateral margins of the vulva to block the terminal branches of the ilioinguinal and genitofemoral nerves. [Fig 22]
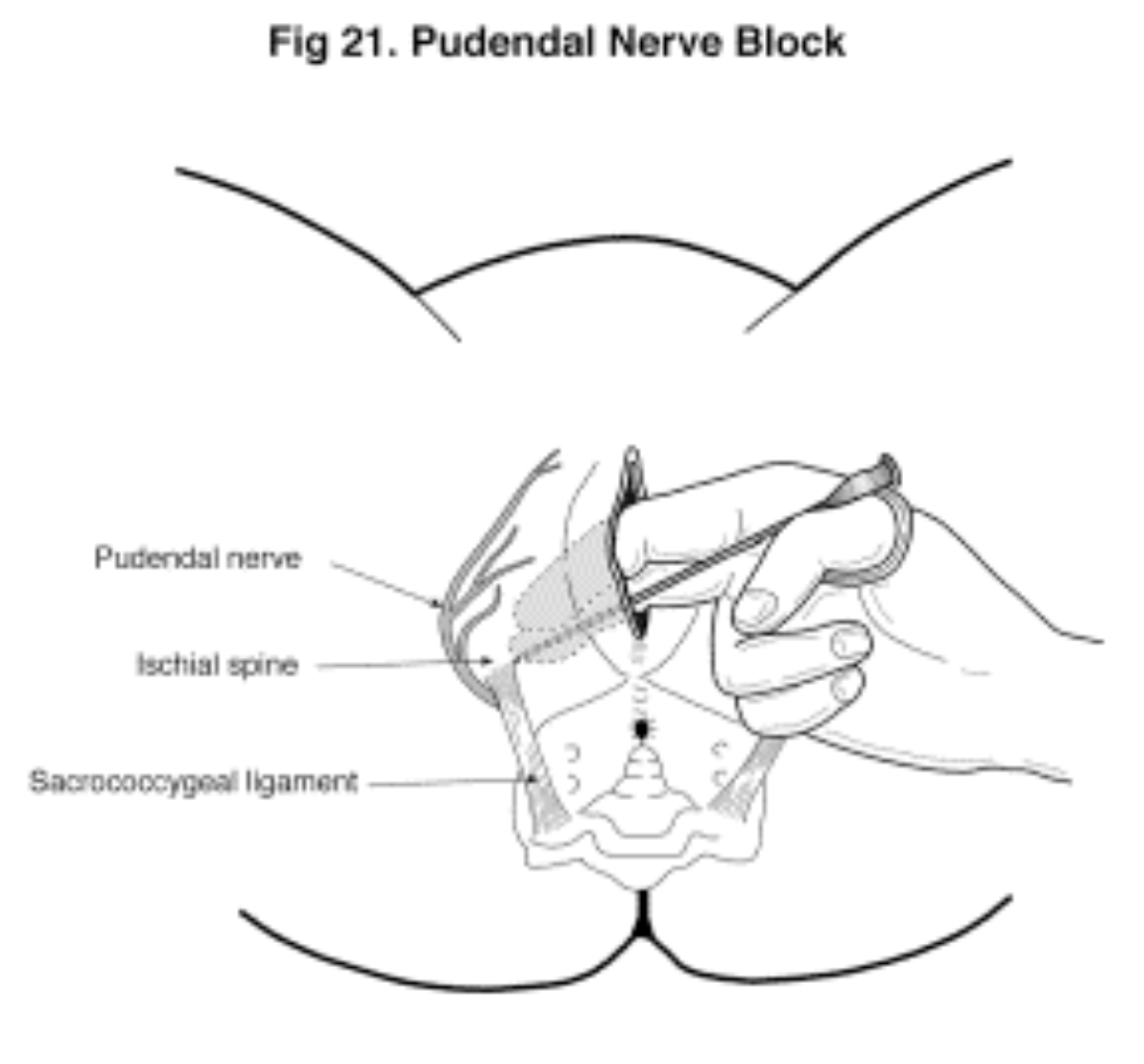
Figure 21 (Click to enlarge)
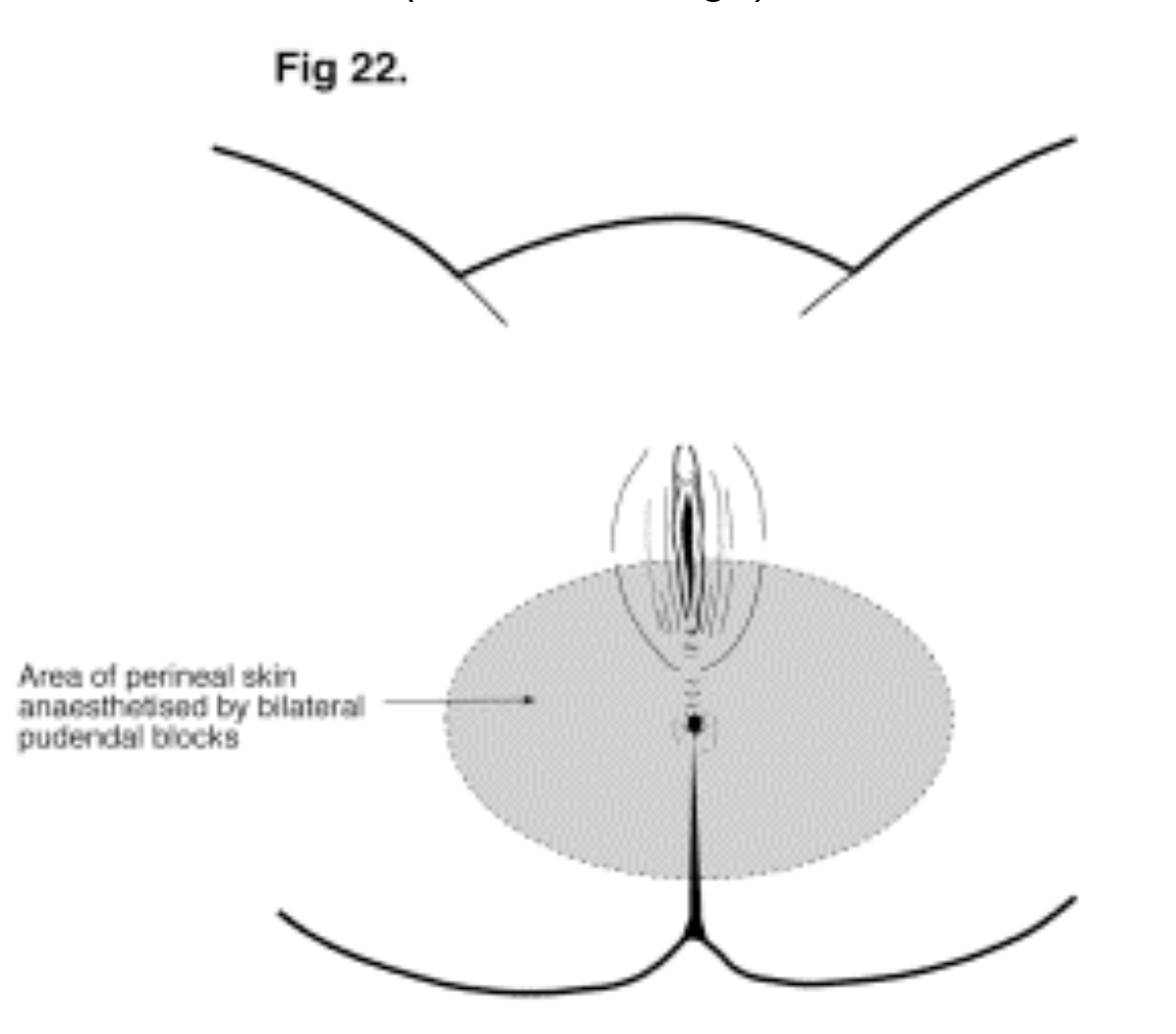
Figure 22 (Click to enlarge)
DRUGS
- For a rapid onset block use lidocaine 1% with epinephrine 1:200,000. Use 10 ml for each nerve and 10 – 15 ml for the subcutaneous infiltration. This should last at least an hour.
- If there is no urgency use bupivacaine 0.25% or ropivacaine 0.4%. A common practice is to mix lidocaine and bupivacaine in a 50:50 ratio.
IMPORTANT POINTS
- This is a very safe block as far as the foetus is concerned but there can be maternal complications.
- Sciatic nerve block: A partial block occurs in 3% of cases. It is usually of no significance and is transient.
- Vaginal haematoma: Uncommon and usually of no consequence.
- Abscess: Uncommon but can invade the ischiorectal fossa.
- Intravascular injection: Always check aspirate and keep the needle tip moving during subcutaneous infiltration.
CONCLUSION
- The pudendal block is known as “The Obstetricians Block” . In expert hands can only expect an 80 % success rate (for bilateral block).
- This block is only suitable for outlet forceps and episiotomies.
- Mid cavity forceps and rotational forceps require an epidural or subarachnoid block.
- The advantage of the pudendal block is that it is easy to perform and has a rapid onset.
- It is ideal for women who have requested natural childbirth but need rescue analgesia in the second stage.



