Paediatric Anaesthesia
KEY POINTS
- Button battery ingestion is a medical emergency; management is incumbent on timely recognition and appropriate imaging.
- Life-threatening complications can occur in less than 2 hours following ingestion of button batteries.
- Oesophageal impaction is most likely in children younger than 6 years and with batteries greater than 20 mm in diameter. These have the highest risk of complications.
- Oesophageal injury may require airway protection, mobilisation of multiple teams, preparation for major haemorrhage, techniques to mitigate further injury, endoscopy and transfer to an appropriate centre.
- Potentially fatal injury can occur weeks after the removal of a button battery from the oesophagus.
- Prevention strategies include raising public awareness, liaising with industry to provide appropriate safety warnings and developing safer battery compartments in products.
INTRODUCTION
The growing presence of domestic electronic equipment has led to an increase in button battery (BB) ingestions in the paediatric population, with associated morbidity and mortality. Remote controls, games and toys are most frequently implicated.1 Impacted batteries can cause ulceration, perforation and fistula formation within hours, possibly leading to severe complications and even death.
The incidence of BB ingestion was just under 11 per million in the United States in 2019, of which the majority (53%) were in children younger than 6 years, indicating that this is the highest-risk age group. Of BB ingestions, 2.8% experienced moderate complications, severe complications or death, with only 3 deaths.2 Those at increased risk of ingestion also include older children with learning difficulties, who may persist in swallowing small objects. A 7-fold increase in relative risk of severe morbidity secondary to BB ingestion in the past 20 years has been reported.3
This has led to prevention initiatives, such as that from the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN).4 Worldwide, working groups, task forces, as well as the families of affected individuals have campaigned for safety standards around BBs to be established in consumer law, for example, in the United States (Reese’s law, August 2022).5
In the United Kingdom, NHS England published a Patient Safety Alert6 in 2014 following cases involving delays in the recognition and treatment of BB ingestion in children (5 cases of severe injury over a 4-year period, with 1 death). ENT UK also published a consensus guideline in 2019.7 The British Paediatric Surveillance Unit are undertaking a national study to investigate the incidence, interventions, complications and outcomes following BB ingestions in children, to better inform clinical care, prevention measures and policy.8 From a legal perspective, the Office for Product Safety and Standards have produced a guidance for businesses that manufacture, import, distribute or sell any products that use button batteries.9
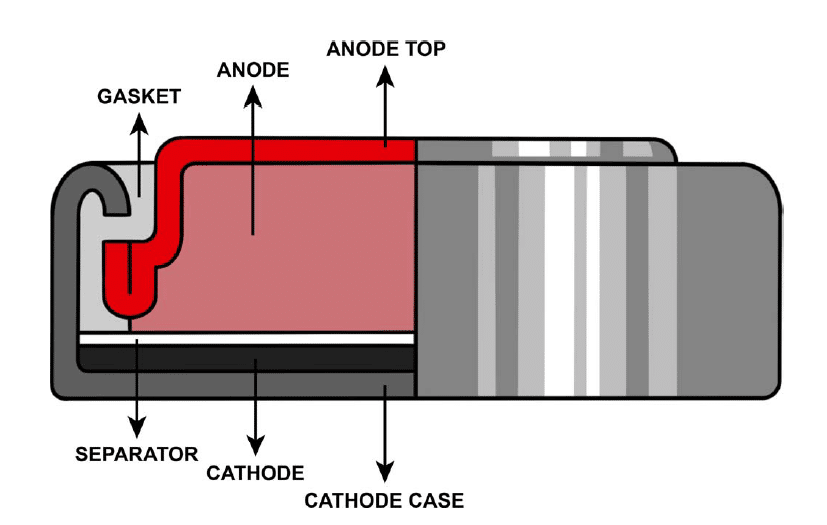
Figure 1. Cross section of a typical button battery (original illustration by Dr Petra Korlevi’c, staff scientist, Wellcome Sanger Institute, Cambridge, UK).
BUTTON BATTERIES
A battery is a series of electrochemical cells in which a chemical reaction generates a potential difference and drives charged particles to flow through a medium, thereby producing an electrical current. Button batteries are single electrochemical cells that generate a potential difference through an oxidation reaction that releases electrons at the anode (negative electrode) and a reduction reaction that absorbs electrons at the cathode (positive electrode). An electrolyte separator connects the electrodes and carries the current through the battery (Figure 1). The most common battery types are L (alkaline battery), S (silver-oxide battery) and C type cells (lithium battery).
More sophisticated battery production has resulted in higher-voltage lithium cells (3 V compared with 1.5 V). These batteries can cause injury even when they are apparently ‘dead’ and no longer able to power a piece of equipment, as they retain residual voltage. The newer cells are also larger than 20 mm in diameter and hence more likely to become impacted in the oesophagus. Moreover, BBs with a diameter greater than 20 mm were more commonly associated with serious complications in children.10
MECHANISM OF INJURY
When ingested and impacted, the 2 poles of the battery are in contact with the surrounding mucosa. This completes a circuit and, as per Ohm’s Law, the large surface area results in a low-resistance circuit with a high current flow through the mucosa. Hydroxide (OH-) ions are produced at the anode, and, as with alkaline liquid ingestion, a caustic injury occurs (see Figure 2).
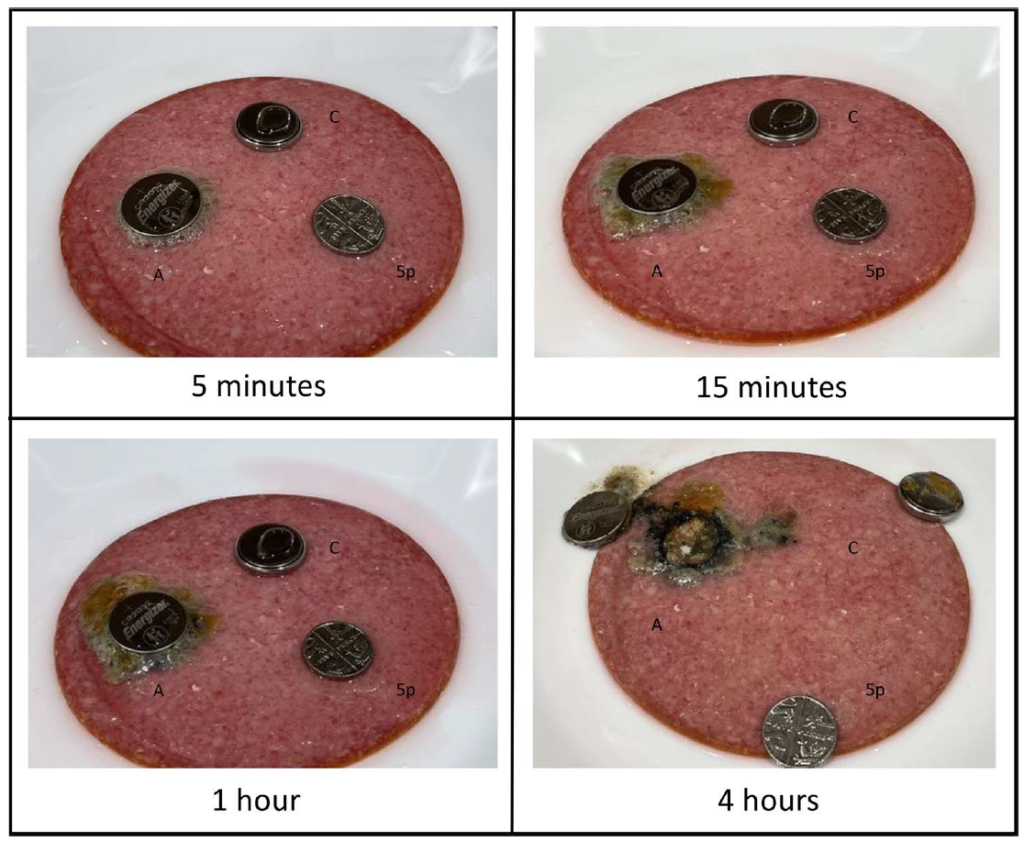
Figure 2. Timeline showing reaction after placement of two 3 V lithium ion button batteries (BBs) and a 5 pence coin on simulated tissue (salami). (A) Anode of 3 V lithium ion BB on simulated tissue. (C) Cathode of 3 Vl Lithium ion BB on simulated tissue. 5p, 5 pence coin on simulated tissue.
The oesophagus is particularly vulnerable to alkaline injury. Acids tend to produce a coagulation necrosis that effectively forms a coagulum, thus limiting tissue penetration. Alkalis, on the other hand, produce a liquefaction necrosis, which penetrates through layers of tissue.11 Given the anatomical proximity of the aerodigestive tract to major blood vessels, the repercussions of tissue liquefaction here (which occurs minutes after OH- production) are profound. Necrosis can lead to oesophageal fistulisation through different planes to the airways, major arteries or the vertebral column.
Complications arising from BB ingestion depend on the location of impaction (Table 1). Some areas are more susceptible to foreign-body retention due to luminal narrowing: the upper oesophagus (C5) due to the cricopharyngeal sling; the mid-oesophagus (T5) due to external compression from the aortic arch, aberrant vessels or the initial portion of the left bronchus; the gastro-oesophageal junction (T10); the pylorus (T12/L1); and the duodenal-jejunal flexure (L2).
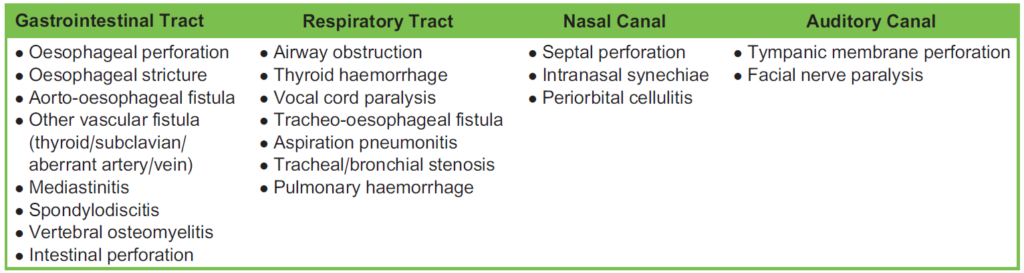
Table 1. Button Battery Complications Based on Site of Impaction
Most complications occur due to injury of the oesophagus (39%), nasal cavity (16%) and the stomach (7%).12 Once they have passed through the pylorus, button batteries are less likely to cause complications13 in part because the mucosa here is relatively robust against alkali.
Children with atypical vasculature, such as an aberrant right subclavian artery, may be at higher risk of catastrophic complications such as arterial-oesophageal fistulae.14 External compression of the oesophagus from this aberrant vasculature can cause narrowing of the lumen, increasing the likelihood of impaction at the level adjacent to the blood vessels, where caustic injury can lead to fatal haemorrhage.
DIAGNOSIS
Unwitnessed ingestions are problematic, not only due to delays in presentation (which could be hours to weeks) but also because the presentation in these cases tends to be with nonspecific symptoms secondary to established complications. Potential ingestion should be considered and investigated without delay in patients with epistaxis, a persistent or atypical croup (a sign of laryngeal oedema), unexplained food refusal, regurgitation, drooling, vomiting in the absence of fever or diarrhoea, respiratory distress, chest or abdominal pain or gastrointestinal bleeding.4
If ingestion is suspected, plain anteroposterior radiographs of the neck, chest and abdomen are immediately indicated. A lateral view radiograph may also provide some information regarding the position of the narrower anode, the most dangerous pole of the BB. Skull radiographs are indicated if there are concerns about nasal or aural insertion and pelvic radiographs if suspicion of rectal or vaginal insertion.4
BBs may appear similar to coins on radiographs; discerning radiologic findings are the presence of a ‘halo’ or ‘double ring’ on a posterior anterior view (high specificity but low sensitivity, as not all button batteries show this feature) or ‘step off’ appearance on lateral view (Figure 3).4 Therefore, any radiographic findings that are suspicious for BB ingestion warrant immediate attention.
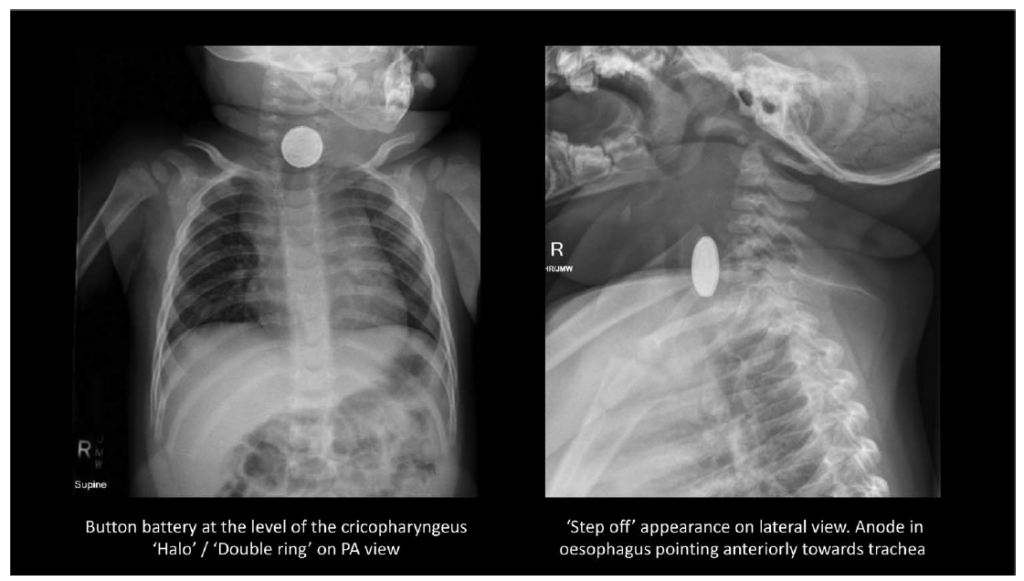
Figure 3. One-year-old male presenting with irritability, cough and rhinorrhoea. Case courtesy of Dr David Chang, Radiopaedia.org, rID: 61397 with permission.
Given the emergent nature of BB ingestion, it is imperative that hospitals have local protocols in place for the diagnosis and management when these are suspected, as exemplified in the ESPGHAN position paper.4 Indeed, the British Association of Paediatric Surgeons in the United Kingdom are currently developing a national guidance document specifically for the ingestion of button batteries and magnets. In our region (east of England), the Operational Delivery Network have produced a regional guideline for the management of suspected or known foreign-body ingestion in children aged 0 to 15 years15 and includes region-specific pro- tocols and contact details. An excerpt specifically addressing BB ingestion is shown in Figure 4.
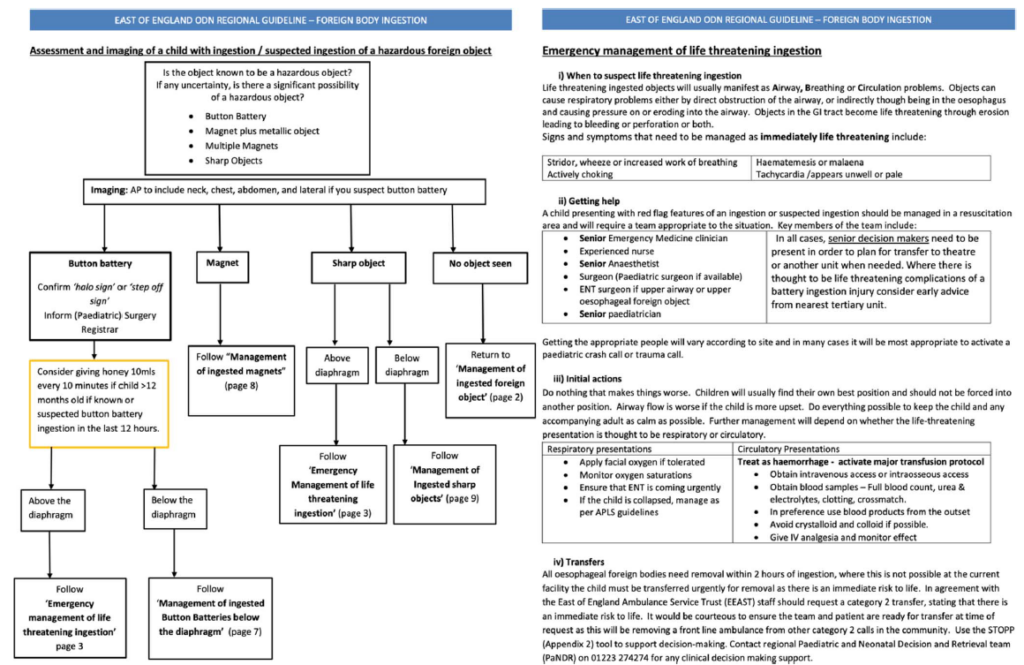
Figure 4. Algorithm for assessment and management of button battery ingestions. East of England ODN Regional Guidelines—Foreign Body Ingestion, Kulkarni M, et al (2023) with permission of East of England Ingested Foreign Body Working Group.
MANAGEMENT
The management depends on the location of the battery, symptoms and time from ingestion. It is imperative that appropriate local protocols are already in place to facilitate communication and decision making in what is potentially a life-threatening emergency.
In the Oesophagus
A BB in the oesophagus within 12 hours since ingestion requires urgent endoscopic removal. The European and North American guidelines state that these should be ideally removed less than 2 hours after ingestion. This is an ambitious target as it would not only include immediate recognition by parents and medical staff but also include transfer to an institution with the appropriate staff and resources, including paediatric cardiac bypass facilities.4
A delayed diagnosis in these cases needs to be approached with extreme care as severe oesophageal injury may already be established. Patients with a delayed diagnosis (more than 12 hours since ingestion) or with symptomatic evidence of serious complications (e.g., haematemesis) may require computed tomography imaging to ascertain the presence and extent of vascular involvement and plan management. In these cases, attempted removal of the BB may lead to acute perforation or catastrophic haemorrhage, and so liaison with a cardiothoracic centre is vital.4
Beyond the Oesophagus
An impacted BB may cause tissue injury and then subsequently pass further along the gastrointestinal tract. As such, clinicians must maintain a high index of suspicion even if the battery is beyond the oesophagus on initial imaging. Regardless of the position of the BB, a symptomatic child, particularly with life-threatening features of stridor, wheeze, increased work of breathing, choking, haematemesis, melaena, epistaxis or tachycardia warrants resuscitation, mobilisation of an appropriate senior team and transfer to theatre for endoscopic retrieval to theatre or an appropriate unit.15
If the BB is in the stomach, the time from ingestion is less than 12 hours and the child remains asymptomatic, they may be monitored. A repeat chest radiograph can be performed to ensure movement along the GI tract. Nearly three-quarters of ingested batteries pass spontaneously within 4 days, and 99% pass within 7 to 14 days.16 If this has not occurred, the upper GI or endoscopy team can remove the battery. Surgical intervention is, fortunately, rarely required.17
Appropriate counselling of guardians, with advice to present immediately if symptoms occur, is critical in these scenarios. Oesophageal damage may already have occurred and manifest even if the BB has passed down into the stomach. Fistulisation may occur up to 28 days postingestion due to residual alkali or weakened, damaged tissue.17
Implications for the Anaesthetist
For oesophageal and/or symptomatic presentations, interventions are warranted regardless of fasting status. A nasogastric tube to aspirate stomach contents (in preparation for a rapid sequence intubation) should not be passed due to the risk of further trauma to the oesophagus. While the appropriate teams are being mobilised, and the patient is perhaps being transferred to a more appropriate centre, it is vital to prepare for potential major haemorrhage and secure the airway via rapid sequence induction.
Pre-endoscopy interventions to reduce the risk of caustic injury to the oesophagus may be used. In children older than 1 year, 10 mL (or 2 spoonfuls) of honey can be given every 10 minutes for up to a maximum of 6 doses (younger children are at risk of botulism). The honey acts as a viscous liquid coating the battery, limiting electrolysis and the production of OH- ions. It is also a weak acid and can help neutralise the pH. In hospital settings, 10 mL of 1 g/10 mL suspension of sucralfate can be used instead, up to 3 doses.18 It is important to note that these interventions must never delay endoscopy, which is the definitive management strategy.
During endoscopy, the mucosa should be carefully inspected for injury, especially at the site in contact with the anode. In certain cases, the endoscopy may be performed in a cardiac catheter lab where angiography can allow visualisation of the BB in relation to blood vessels. A nasogastric tube can cause further trauma to a friable oesophagus and should be placed only by the endoscopist under direct vision. This prevents further injury from feeding and allows healing.4 After removal of BB, the oesophagus is carefully examined. If satisfied with the integrity of the oesophagus, further neutralisation of residual OH- ions can be done during the endos- copy by irrigating with 0.25% acetic acid.17
Postoperatively, children with mucosal injury may be monitored in a high-dependency setting. Depending on the extent of injury, a second-look endoscopy between 2 and 4 days postremoval may be considered.13 Intravenous antibiotics and steroids may be indicated only if there are concerns regarding mediastinitis. Feeding and a long-term follow-up plan will be dictated by the findings at endoscopy and evolution of complications. Antacids may be used at the discretion of local teams to prevent further injury to the oesophagus, but there is no evidence for, or against, this.17
Discharge instruction for patients who have suffered severe oesophageal injury needs to emphasise signs and symptoms of upper GI bleed as it can takes weeks for nonviable tissue to manifest. Most fatal haemorrhages from aorto-oesophageal fistula take place after battery removal; sentinel bleeds herald exanguination.12 Patients may also be followed up in the long term to assess for development of strictures.
SUMMARY
BB ingestion is a medical emergency, which may present insidiously with nonspecific signs. Every institution should be prepared for this presentation, with context-specific protocols or pathways to aid rapid diagnosis, mobilisation of relevant team members and endoscopic removal in a timely manner. Preintervention mitigation with honey and sucralfate must never delay imaging or definitive removal of battery in endoscopy. Injury to structures around the oesophagus can complicate management and must be prepared for. Once the BB is removed, the child should be closely monitored for progression of oesophageal injury.
REFERENCES
Litovitz T, Whitaker N, Clark L, et al. Emerging battery-ingestion hazard: clinical implications. Pediatrics. 2010;125:1168-1177.
National Capital Poison Centre. Poison control 2021. Accessed February 1, 2023. https://www.poison.org/battery/stats#table2
Eliason M, Ricca R, Gallaghe T. Button battery ingestion in children. Curr Opin Otolaryngol Head Neck Surg. 2017;25:520-526.
Mubarak A, Benninga MA, Broekaert I, et al. Diagnosis, management, and prevention of button battery ingestion in child- hood: a European Society for Paediatric Gastroenterology Hepatology and Nutrition position paper. Pediatr Gastroenterol Nutr. 2021;73(1):129-136.
United States Committee on Energy and Commerce, H.R. 5313, 117th Congress (2021-2022): Reese’s Law. Accessed August 20, 2023. https://www.govinfo.gov/app/details/BILLS-117hr5313ih
NHS England. Patient safety alert: risk of death and serious harm from delays in recognising and treating ingestion of button batteries. December 2014. Accessed February 1, 2023. https://www.england.nhs.uk/2014/12/psa-button-batteries/
Houston R, Powell S, Jaffray B, et al. Clinical guideline for retained button batteries. Arch Dis Childhood. 2021;106:192-194.
Basu S; British Paediatric Surveillance Unit, Royal College of Paediatric and Child Health. Button battery ingestion, inhala- tion or insertion. Accessed February 20, 2023. http://www.rcpch.ac.uk/bpsu/button-battery-ingestion
United Kingdom Office for Product Safety and Standards. March 2022. Accessed December 15, 2022. https://www.gov.uk/ guidance/using-button-and-coin-batteries#legal-requirements
Krom H, Visser M, Hulst J, et al. Serious complications after button battery ingestion in children. Eur J Pediatr. 2018;177:1063-1070.
Hall AH, Jacquemin D, Henny D, et al. Corrosive substances ingestion: a review. Crit Rev Toxicol. 2019;49(8):637-669.
Varga A, Kovacs T, Saxena AK. Analysis of complications after button battery ingestion in children. Pediatr Emerg Care. 2018;34:443-446.
Ruhl D, Cable B, Rieth K. Emergent treatment of button batteries in the oesophagus: evolution of management and need for close second look esophagoscopy. Ann Otol Rhinol Larynol. 2014;123:206.
Fuentes S, Cano I, Benavent MI, Go´mez A. Severe esophageal injuries caused by accidental button battery ingestion in children. J Emerg Trauma Shock. 2014;7(4):316-321.
East of England Ingested Foreign Body Working Group. 2023. East of England ODN regional guideline—foreign body ingestion. Accessed September 1, 2023. https://www.eoeneonatalpccsicnetwork.nhs.uk/wp-content/uploads/2023/08/Pae diatric-Foreign-Body-Ingestion.pdf- Litovitz T. Battery ingestions: product accessibility and clinical course. Pediatrics. 1985;75:469-476.
Lerner D, Brumbaugh D, Lightdale J. Mitigating risk of swallowed button batteries: new strategies before and after removal. J Pediatr Gastroenterol Nutr. 2020;70:542-546.
Anfang RR, Jatana KR, Linn RL, Rhoades K, Fry J, Jacobs IN. pH-neutralizing esophageal irrigations as a novel mitigation strategy for button battery injury. Laryngoscope. 2019;129:49-57.



