Obstetrics Anaesthesia
KEY POINTS
- Heart rate (HR) and blood pressure (BP) are crude surrogate markers for cardiac output (CO).
- CO ¼ HR 3 SV, and CO is also related to BP and systemic vascular resistance (SVR), as demonstrated by the equation CO ¼ BP/SVR.
- Minimal, noninvasive CO monitoring is preferable to invasive techniques in awake patients.
- CO monitoring is particularly helpful in certain circumstances (eg, pregnant patients with preeclampsia with severe features, massive haemorrhage, or cardiomyopathy).
INTRODUCTION
In routine clinical practice, heart rate (HR) and blood pressure (BP) are surrogate markers for cardiac output (CO), oxygen delivery and tissue perfusion. Although relatively crude, these easily obtainable parameters routinely guide clinical decision making in healthy pregnant and postpartum patients. There are numerous CO-monitoring techniques that play an evolving role in haemodynamic assessment of patients undergoing major surgery or in the critical care environment. When caring for an awake critically ill obstetric patient, there may be a conflict between the need for accurate CO monitoring to guide therapy and maintaining a minimally invasive approach.
This tutorial summarises haemodynamic changes in pregnancy and discusses current evidence for various noninvasive and minimally invasive CO-monitoring techniques.1
HAEMODYNAMIC CHANGES IN A PREGNANT PATIENT AND RELEVANCE TO OBSTETRIC ANAESTHESIOLOGY
The metabolic demands of the growing foetus and placenta drive the cardiovascular adaptations of pregnancy. In the absence of heart disease, maternal physiology adapts efficiently to increased demands, increased circulating blood volume, reduced systemic vascular resistance (SVR) and increased myocardial contractility and HR (Table 1).2 However, in patients with a known heart condition or undetected (prior to pregnancy) reduced cardiac reserve, the increased cardiovascular work of pregnancy can result in maternal decompensation.
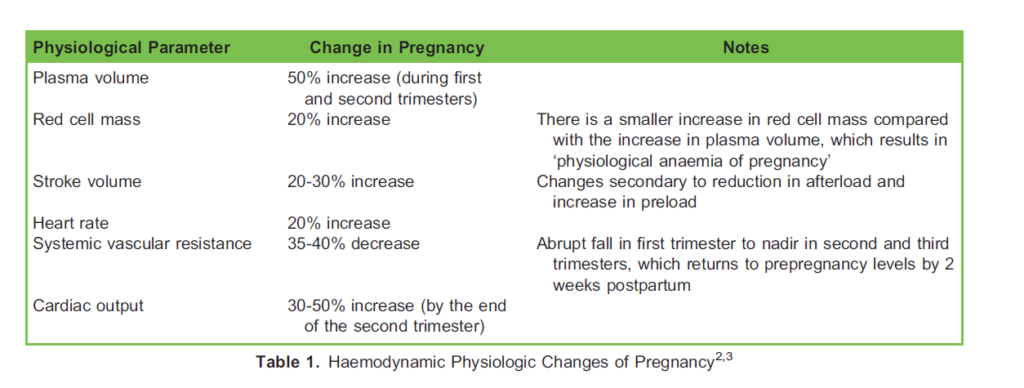
In addition to the gradual physiological adaptations of pregnancy, additional haemodynamic changes occur at the time of labour and delivery. Uterine contractions will intermittently increase central blood volume by up to 500 mL, increased circulating catecholamines (eg, from labour pain) increase the maternal HR, and immediately postdelivery, decompression of the inferior vena cava and autotransfusion result in a further increase in CO by as much as 80% from prelabour values.4 These increases in CO, HR and BP may result in decompensation (eg, failure) in a system that had previously been compensating. Patients who are unable to increase CO (eg, those with aortic stenosis) may develop symptoms or signs of left or right heart failure, and increased cardiac work and myocardial oxygen consumption may trigger cardiac ischaemia.
METHODS OF NONINVASIVE AND MINIMALLY INVASIVE CO MONITORING IN PREGNANCY
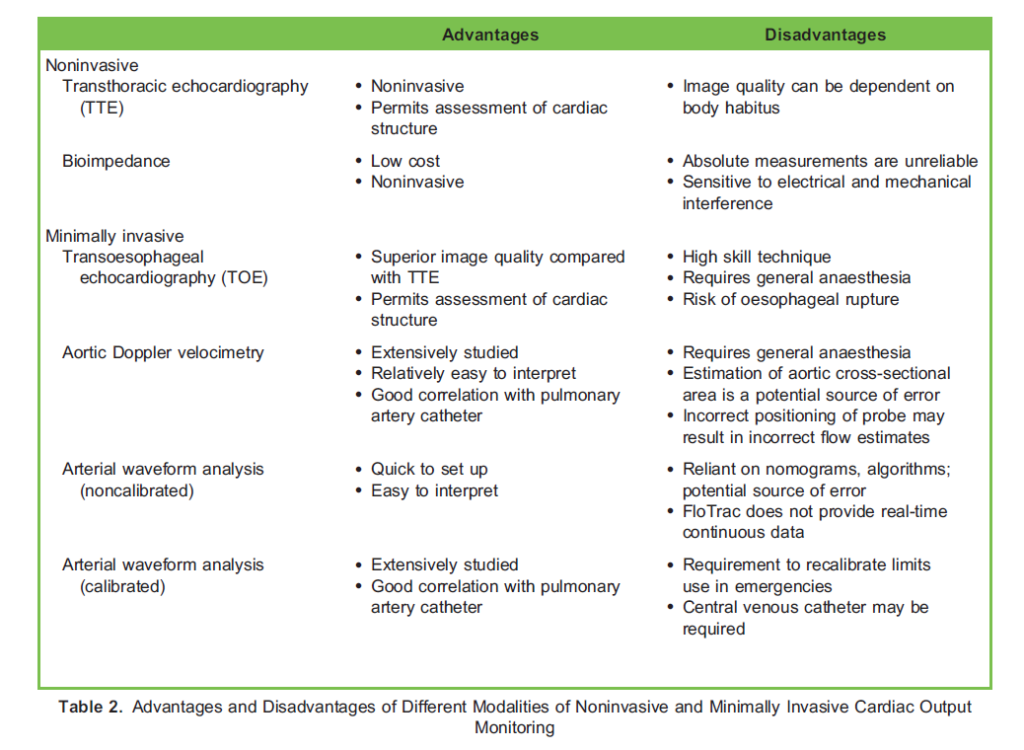
There are various techniques and devices that use different technologies and measure a range of physiological parameters to calculate CO. The choice of monitor depends on availability, ease of use, accuracy and precision, and there are advantages and disadvantages, which are summarised in Table 2.
Transthoracic and Transoesophageal Echocardiography
Transthoracic echocardiography (TTE) and transoesophageal echocardiography (TOE) measure the flow at the LV outflow tract, ascending aorta, main pulmonary artery, right ventricular outflow tract and across the mitral valve. Both methods are able to assess haemodynamic variables (eg, cardiac filling status and contractility) as well as anatomical structure. There is excellent correlation between echocardiographic and thermodilution techniques in nonpregnant patients.5 TTE is a noninvasive and safe method for assessing cardiac structure and function. TOE provides clearer images than TTE because of the reduction in signal attenuation by the chest wall, but it must be performed under sedation or general anaesthesia. Thus, because most obstetric cases are performed under neuraxial anaesthesia, TOE is less suitable in routine obstetric cases. Although interest is increasing in these methods, TTE and TOE are not common skills amongst obstetric anaesthetists and are not suitable for the occasional user in an emergency.
Aortic Doppler Velocimetry
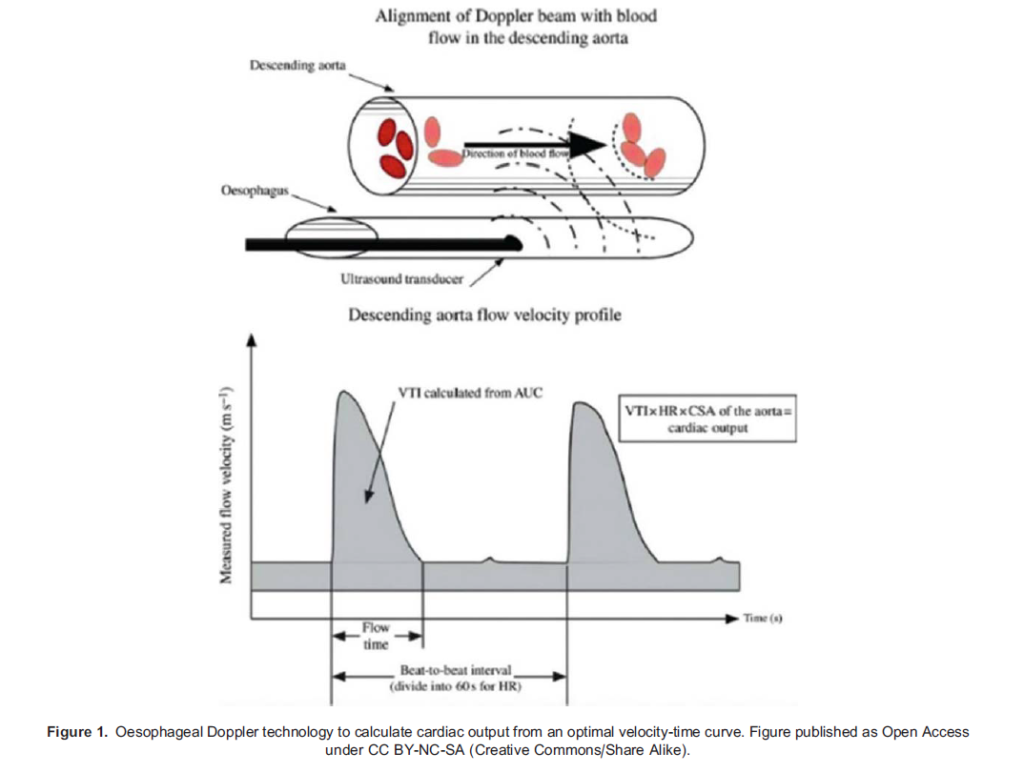
Doppler velocimetry utilises the Doppler shift principle to calculate the velocity of red blood cells. The oesophageal technique measures blood velocity in the descending aorta. The cross-section of the aorta is estimated from nomograms based on age, weight and height. A velocity-time graph is displayed, and an integral of the derivative of velocity-over-time is multiplied by the cross-sectional area to give a value for stroke volume (SV). This technique is not tolerated in the awake patient, and it assumes that the aortic size is constant (Figure 1).
The suprasternal Doppler, which was developed using Doppler velocimetry technology, is a noninvasive technique that uses a Doppler probe placed in the suprasternal notch. Individual devices aim to study either the descending aortic arch or the aortic and pulmonary outflow tracts. Commercially available devices include the SupraQ Cardiac Function Monitor (Deltex Medical, Chichester, UK) and the ultrasonic CO monitor (USCOM; Uscom Ltd., Sydney, Australia). The SupraQ Cardiac Function Monitor aims for the descending aortic arch, while the USCOM targets the aortic/pulmonary outflow tracts. These techniques have been shown to have reasonable agreement with the pulmonary artery catheter and have been used in several clinical studies to measure cardiovascular response in healthy pregnant patients.7,8
Bioimpedance
Bioimpedance is a simple, low-cost, easy-to-use noninvasive technique that detects electrical resistance changes across the thorax or whole body induced by changes in vascular flow throughout the cardiac cycle. There have been reports of inaccuracies with this technique, as it may be affected by patient position (and variance in the interelectrode distance), pulmonary oedema, diathermy and mechanical ventilation, which may limit its use in certain situations (eg, in labour and during caesarean delivery (CD)).
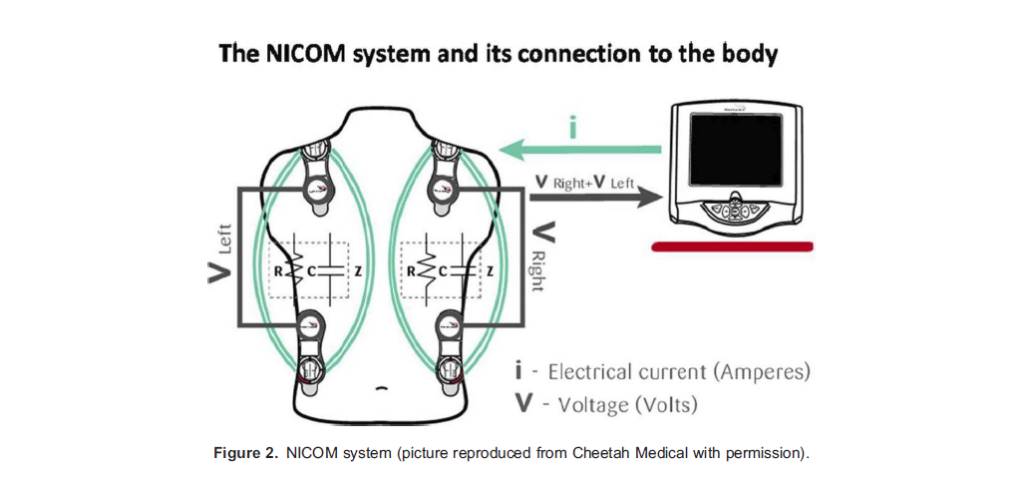
Bioreactance is a technique designed to overcome problems of bioimpedance and involves the analysis of relative phase shifts of oscillating current that occur when traversing the thoracic cavity, improving the signal-to-noise ratio. The noninvasive CO monitor (NICOM; Cheetah Medical, Maidenhead, UK) and AESCULON (Osypka Medical Services, Berlin, Germany) are 2 examples of available devices (Figure 2). There are varying reports of the accuracy of these devices compared with thermodilution techniques, and it is suggested that they are more suited to displaying trends in CO and changes with interventions rather than for one-off measurements.6
Arterial Waveform Analysis
Pulse contour analysis uses the waveform derived from an invasive arterial line to predict vascular flow. It is based on the general principle that the amplitude of the systolic part of the arterial curve is proportional to CO and arterial compliance and has the advantage of being continuous and in real time. Calibrated devices (in which the initial estimation of CO by pressure waveform analysis is calibrated by measurements of CO made by transpulmonary thermal or lithium dilution) include LiDCOplus (lithium dilution CO; LiDCO Ltd., London,UK) and PiCCO (pulse index contour continuous CO; Pulsion Medical Systems, Feldkirchen, Germany). Noncalibrated devices include the LiDCO-rapid, FloTrac (Edwards Lifesciences Corp., Irvine, CA, USA) and Nexfin (BMEYE, Amsterdam, the Netherlands). These devices have significant advantages for the obstetric anaesthetist, as they are minimally invasive (as long as an arterial line is in situ) and are simple to set up for the occasional user; however, waveform damping and/or siting an arterial catheter in a small distal vessel (eg, dorsalis pedis artery) will impair the accuracy of the data.
Calibrated Arterial Waveform Analysis
LiDCO-plus uses lithium dilution calibration to give an accurate baseline measurement for SV. CO is derived from the area under a concentration-time curve using the Stewart-Hamilton equation. LiDCO-plus has been used in understanding the pathophysiology of diseases such as preeclampsia, but it has been suggested that it is unlikely to be appropriate in situations of acute haemodynamic fluctuations such as during CD; measurement of CO during rapid changes in cardiovascular variables are unreliable and prone to significant error.9
PiCCO employs transpulmonary thermodilution for measurements of absolute CO and pulse contour, rather than pulse pressure analysis to generate beat-to-beat CO. It allows estimation of variables such as intravascular lung volumes and extravascular lung water. It requires a central venous catheter and peripheral arterial line with regular calibration, which may preclude its use in regular obstetric practice; however, it may be applicable for use in a critically ill obstetric patient.1 A PubMed search using keywords ‘PiCCO’, ‘Obstetrics’, ‘Pregnancy’ and ‘Caesarean’ yielded no results.
Noncalibrated Arterial Waveform Analysis
The FloTrac sensor uses a statistical analysis of 20-second windows of radial artery pressure waveforms in conjunction with estimates for compliance and incorporates patient demographics into its calculations; however, it does not give true continuous real-time data.1 Studies have demonstrated good correlation with thermodilution in stable patients and the ability to predict fluid responsiveness in patients with septic shock with reasonable accuracy.10 Variable results have been found in attempting to accurately track changes in haemodynamically unstable patients, which suggests caution should be exercised when using this device in patients on vasopressor or inotropic support or in environments where there may be rapid haemodynamic changes such as during CD.6
The LiDCO-rapid system uses the same algorithm as the LiDCO-plus to derive SV and HR from the BP waveform. This algorithm uses nomograms to predict the aortic compliance for an individual patient using demographic characteristics that do not change over the short term. The LiDCO-rapid system has been used successfully in a number of obstetric studies, both research-based and clinically.
The Nexfin monitor is a noninvasive monitor that uses an inflatable cuff around the middle phalanx of the finger to derive the finger arterial pressure waveform, from which a brachial pressure arterial waveform is constructed. A specific pulse contour analysis based on the pressure area of the waveform and an individualised Windkessel model for each patient is used to derive CO.
WHY AND WHEN CAN WE USE CO MONITORING IN PREGNANT PATIENTS?
Research in Healthy Pregnant Patients
There have been a number of studies using CO monitoring, highlighting its usefulness for research purposes in the healthy pregnant patient, particularly in understanding spinal-induced hypotension and the response to fluid loading and vasopressors.
Meirowitz et al. using NICOM, demonstrated that a positive SV response to a passive leg raise is not predictive of spinalinduced hypotension.11
Xiao et al. used LiDCO-rapid to demonstrate that a goal-directed fluid protocol in healthy pregnant patients was associated with a lower incidence of spinal-induced hypotension, a lower total phenylephrine dose (administered by boluses) and a favourable neonatal cord gas result.12
Disease States
Preeclampsia
Pulse waveform analysis and suprasternal Doppler have been useful research tools in establishing CO changes associated with spinal anaesthesia in healthy and preeclamptic women and also to guide the use of fluid, vasopressors and oxytocin administration during spinal anaesthesia.13 Following administration of oxytocin, a proportion of women with severe preeclampsia and possible diastolic dysfunction respond with a decrease in SV and CO, and these findings reinforce the recommendation that oxytocin should be administered slowly, especially in patients with severe disease. This work has served as a guide for phenylephrine dosing and the use of HR as a surrogate marker for CO changes during spinal anaesthesia for CD.
Cardiac Disease
In the absence of preexisting heart disease, peripartum cardiomyopathy (PPCM) typically presents in the last 4 weeks of pregnancy and up to 5 months postpartum, and mortality may exceed 10%.14 PPCM is characterised by LV dysfunction (eg, LV ejection fraction ,45%) and is associated with congestive cardiac failure, arrhythmia(s), intracardiac thrombus and sudden cardiac death. Echocardiography in particular is a very effective tool for diagnosis and management of cardiac disease, and cardiomyopathy in pregnancy is no exception. This situation was described in a case report, in which TTE was used to diagnose PPCM, revealing significant LV dilatation and reduced contractility in a previously healthy 31-year-old nulliparous patient at 35 weeks of gestation.15 In addition, NICOM has been used during labour and delivery as an adjunct to clinical examination to allow estimation of fluid status and guide titration of epidural analgesia.15 NICOM is of particular benefit as it is noninvasive, and unlike TTE it provides continuous monitoring of CO and associated haemodynamic variables to allow for the early detection of any reduction in afterload and SVR with neuraxial anaesthesia.15
Massive Obstetric Haemorrhage
Management of massive obstetric haemorrhage (MOH) requires volume resuscitation with intravenous fluids and blood products. CO monitoring not only assists in directing fluid management but may also discriminate between hypovolaemia and cardiac impairment, thus guiding the use of inotropic drugs and vasopressors where indicated. Schiralidi et al. described a case of CD complicated by MOH in which oesophageal Doppler was used to monitor and guide fluid therapy, titrate noradrenaline and reduce the premature addition of further inotropic support in a hypovolaemic patient.16
CO monitoring may be particularly helpful in guiding therapy in the setting of a combination of morbidities, for example, preeclampsia with severe features and significant postpartum haemorrhage.
SUMMARY
- Pregnancy imposes significant changes and challenges on the maternal cardiovascular system.
- CO measurement is useful in obstetric anaesthesiology as an adjunct to surrogate markers of CO, although the method chosen should be tailored to the individual situation.
- CO monitoring is particularly helpful in critically ill pregnant patients to improve the understanding of normal physiology, pathophysiology and response to anaesthesiology, fluids, and vasoactive drugs in the clinical settings and in research.
REFERENCES
- Armstrong S, Fernando R, Columb M. Minimally- and non-invasive assessment of maternal cardiac output: go with the flow! Int J Obstet Anesth. 2011;20(4):330-340.
- Bedson R, Riccoboni A. Physiology of pregnancy: clinical anaesthetic implications. Contin Educ Anaesth Crit Care Pain. 2014;14:69-72.
- Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014;130(12):1003-1008.
- Nelson-Piercy C. Heart disease. In: Nelson-Piercy C, Ed. Handbook of Obstetric Medicine. 2nd ed. Abingdon, England: Taylor & Francis Group; 2002.
- Nishimura RA, Callahan MJ, Schaff HV, et al. Noninvasive measurement of cardiac output by continuous-wave Doppler echocardiography: initial experience and review of the literature. Mayo Clin Proc. 1984;59(7):484-489.
- Kobe J, Mishra N, Arya VK et el. Cardiac output monitoring: technology and choice. Ann Card Anaesth. 2019;22(1):617.
- Mon W, Stewart A, Fernando R, et al. Cardiac output changes with phenylephrine and ephedrine infusions during spinal anesthesia for cesarean section: a randomized, double-blind trial. J Clin Anesth. 2017;37:43-48.
- Armstrong S, Fernando R, Columb M, Jones T. Cardiac index in term pregnant women in the sitting, lateral, and supine positions: an observational, crossover study. Anesth Analg. 2011;113(2):318-322.
- Pauca AL. Pressure wave analysis is useful to understand the pathophysiology of preeclampsia, but perhaps not the rapid changes during cesarean delivery. Anesthesiology. 2008;108(5):773-774.
- Krige A, Bland M, Fanshawe T. Fluid responsiveness prediction using Vigileo FloTrac measured cardiac output changes during passive leg raise test. J Intensive Care. 2016;4:63.
- Meirowitz N, Katz A, Danzer B, Siegenfeld R. Can the passive leg raise test predict spinal hypotension during cesarean delivery? An observational pilot study. Int J Obstet Anesth. 2012;21(4):324-328.
- Xiao W, Duan Q, Zhao L, et al. Goal-directed fluid therapy may improve hemodynamic stability in parturient women under combined spinal epidural anesthesia for cesarean section and newborn well-being. J Obstet Gynaecol Res. 2015;41(10):1547-1555.
- Rosseland LA, Hauge TH, Grindheim G, et al. Changes in blood pressure and cardiac output during cesarean delivery: the effects of oxytocin and carbetocin compared with placebo. Anesthesiology. 2013;119:541-551.
- Bhattacharyya A, Basra SS, Sen P, Kar B. Peripartum cardiomyopathy: a review. Tex Heart Inst J. 2012;39(1):8-16.
- Lorello G, Cubillos J, McDonald M, Balki M. Peripartum cardiomyopathy: postpartum decompensation and use of noninvasive cardiac output monitoring. Int J Obstet Anesth. 2014;23(1):66-70.
- Schiraldi R, Calderon L, Maggi G et al. Transoesophageal Doppler-guided fluid management in massive obstetric´ haemorrhage. Int J Obstet Anesth. 2014;23(1):71-74