Regional Anaesthesia
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Please answer True or False: The femoral nerve:
a. Is derived from the dorsal rami of L2 to L4
b. Is covered by 2 fascial layers, the fascia lata and fascia iliaca
c. Is contained within the femoral sheath
d. Emerges from the psoas muscle at its medial border.
e. Divides into anterior (superficial) and posterior (deep) branches after passing under the inguinal ligament - Please answer True or False: The femoral nerve block provides:
a. Sensory block of the skin over the anterior aspect of the lower leg
b. Motor block of the extensor muscles of the knee
c. Sensory block of the skin over the lateral aspect of the hip joint
d. Surgical anaesthesia for skin grafting from the anterior aspect of the thigh
e. Analgesia for all lower leg surgery in combination with sciatic nerve block - Please answer True or False: With regard to the performance of the femoral nerve block:
a. Stimulation of the sartorius muscle implies the needle tip is too lateral
b. The femoral nerve is usually found at the midpoint between the anterior superior iliac spine and pubic symphysis
c. Directing the needle cranially and injecting a volume of 30mls will also result in blockade of the lateral femoral cutaneous and obturator nerves
d. Two distinct ‘pops’ may be felt as the needle is advanced
e. The correct motor endpoint is contraction of the patella
INTRODUCTION
The femoral nerve block is one of the easiest peripheral nerve blocks to master because the landmarks are generally easy to identify and the nerve is usually found at a superficial depth. Historically, the technique was sometimes termed the “3 in 1 block” because it was thought a single injection could block the femoral, lateral femoral cutaneous and obturator nerves. However, although the femoral nerve is reliably blocked, the lateral femoral cutaneous nerve is often missed and the obturator nerve is almost always missed1,2.
The block is usually performed as a single shot, however its duration of action may be extended with a catheter technique. When using a catheter local anaesthetic may be delivered by repeated boluses, patient controlled boluses or continuous infusion. The femoral nerve can be located using ultrasound guidance. This article will only discuss the single shot femoral nerve block performed using a landmark approach. The article will cover relevant anatomy, potential uses and block technique along with a brief trouble shooting section.
ANATOMY
The Femoral nerve
The femoral nerve is the largest branch of the lumbar plexus (Figure 1) and arises from the ventral rami of the second, third and fourth lumbar nerves. It descends through the substance of the psoas major muscle deep to the fascia iliaca emerging from the muscle at its lateral border. It continues caudally into the thigh via the groove formed between the psoas and iliacus muscles and passes under the inguinal ligament to enter the femoral triangle. Here it lies on top of the iliacus muscle lateral to the femoral artery. The femoral nerve lies outside of the femoral sheath and is covered by two fascial layers, the fascia lata and fascia iliaca. The femoral vessels, however, are only covered by a single layer, the fascia lata. Thus the nerve actually lies in a different tissue plane to the vessels.
Immediately after passing under the inguinal ligament, the femoral nerve divides into anterior (superficial) and posterior (deep) branches. Clinically this is important because one of the branches can easily be missed if the block is not performed close to the inguinal ligament. The anterior branch provides motor innervation to the sartorius and pectineus muscles and sensory innervation to the articular surface of the acetabulum and skin of the anterior and medial thigh. The posterior branch provides motor innervation to the quadriceps muscle and sensory innervation via the saphenous nerve. The latter provides the only sensory innvervation below the knee to have originated from the femoral nerve. It supplies the skin over the medial aspect of the leg down to the medial malleolus and descends through the thigh in the adductor canal with the nerve to the vastus medialis muscle.
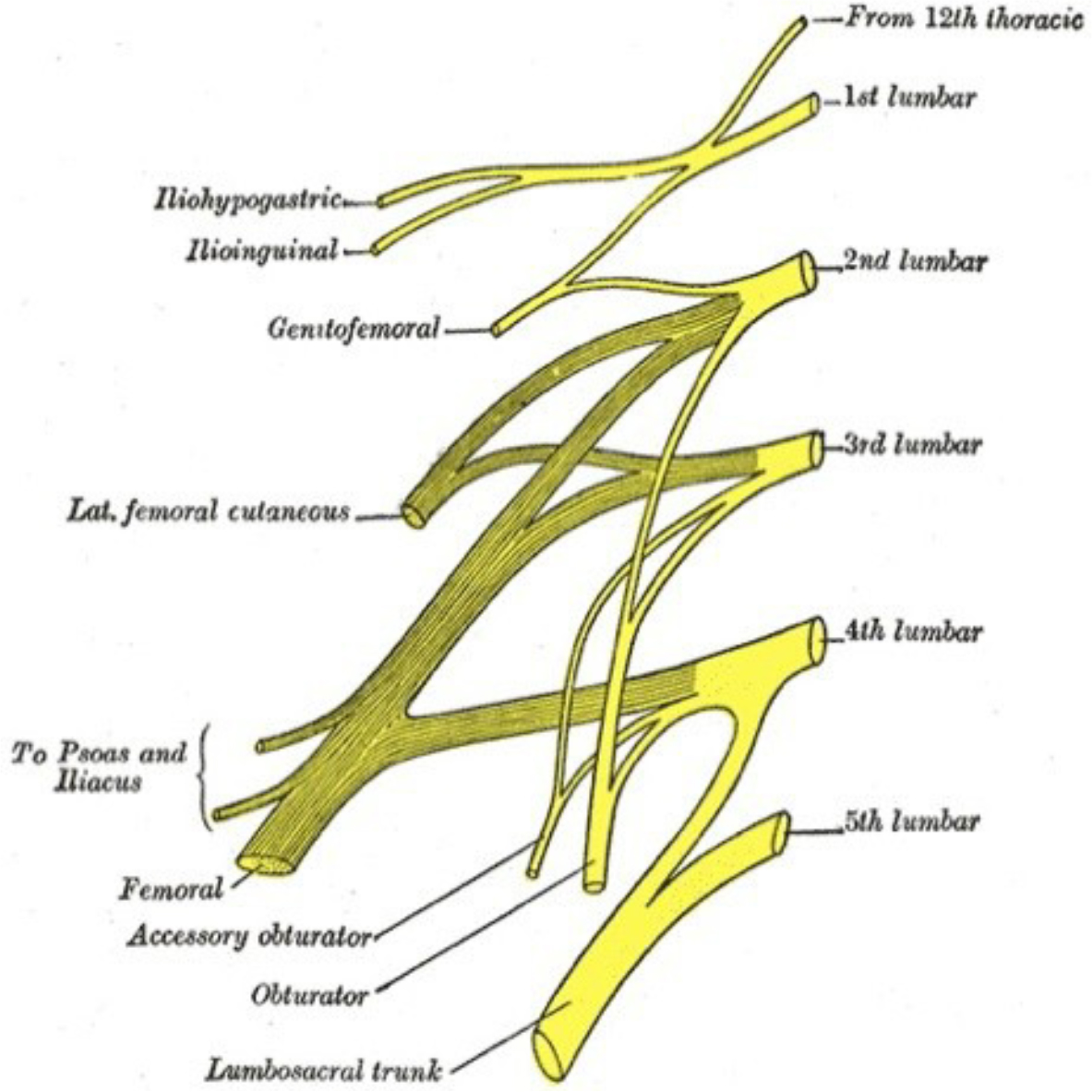
Figure 1. Right Lumbar Plexus. Note the Femoral nerve arising from the 2nd, 3rd and 4th lumbar roots.
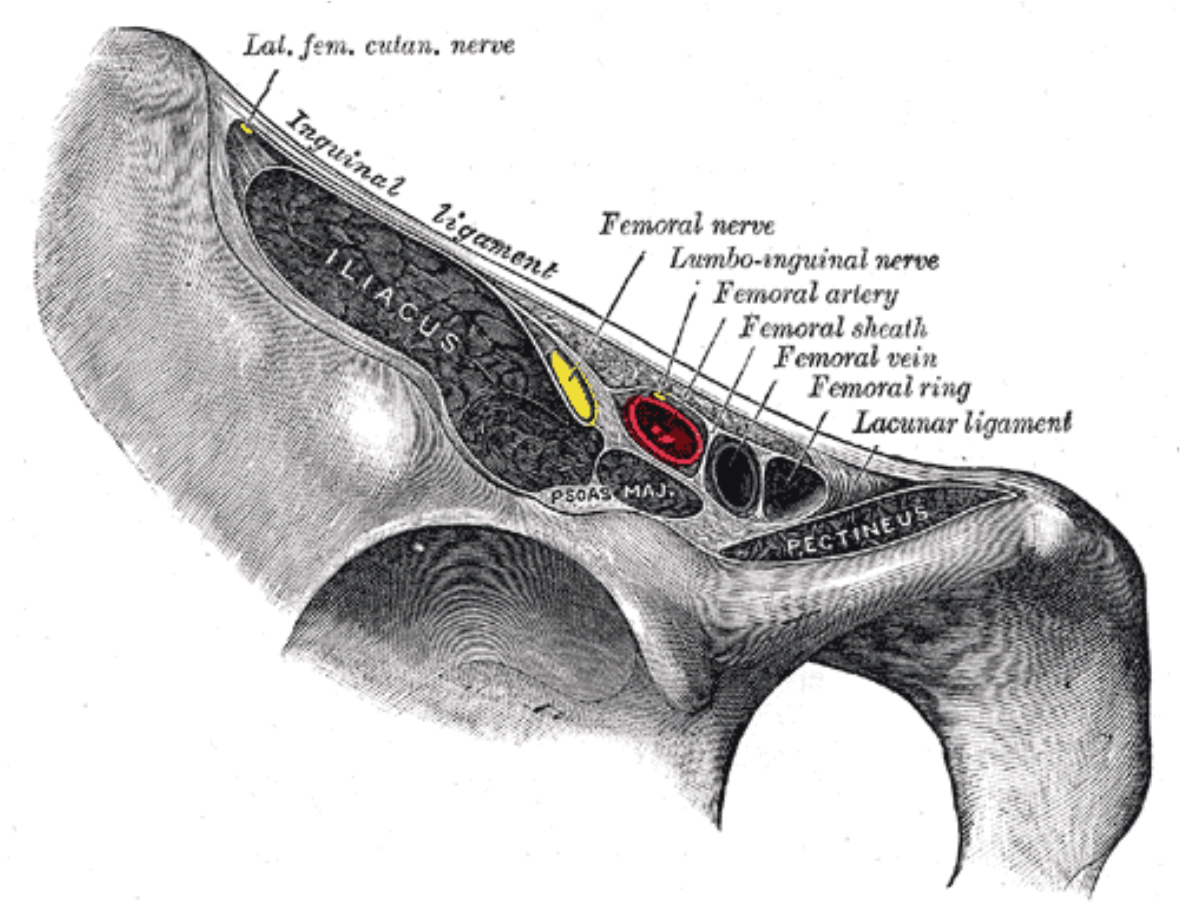
Figure 2. Structures passing under the inguinal ligament. Note the femoral nerve is lateral to the femoral vessels and lies outside the femoral sheath.
Anatomical variations
The femoral nerve may arise from the ventral rami of T12 to L4 (prefixed) or from L1 to L5 (postfixed). Rarely the nerve may be found within the iliopsoas muscle or between the femoral vessels.
Applied Anatomy
Dermatomal innervations
The femoral nerve innervates the skin over the antero-medial aspect of the thigh and knee, and the medial border of the leg and medial malleolus (via the saphenous nerve).
Myotomal innervations
The femoral nerve innervates the following muscles: sartorius, quadriceps femoris (rectus femoris, vastus lateralis, vastus intermedius and vastus medialis), iliopsoas and pectineus.
Osteotomal innervations
The femoral nerve innervates the anterior wall of the hip joint, the anterior aspect of the femur and the anteromedial walls of the knee joint.
INDICATIONS
As with all blocks a FNB can reduce systemic opiate requirements with their side effects. This may be particularly important in the elderly or those with respiratory disease. Thus the femoral nerve block can be performed to provide perioperative analgesia for fractured neck/shaft of femur or postoperative analgesia after knee surgery. It can also be used to provide surgical anaesthesia, usually in combination with a sciatic nerve block. This may be advantageous in situations where it would be preferable to avoid general or neuraxial anaesthesia.
Analgesia
- After knee surgery, for example total knee arthoplasty (with/without sciatic nerve block) or anterior cruciate ligament repair. Please note that in most patients a femoral nerve block alone will not provide adequate analgesia of the knee due to significant contributions from the sciatic and obturator nerves.
- When combined with a sciatic or popliteal block, a femoral nerve block can provide analgesia for above and below knee amputations.
- For plaster applications in children with femoral fracture.
- Perioperative analgesia in fractured neck/shaft of femur (can be useful to facilitate patient positioning prior to neuraxial block).
- Adjuvant analgesia following hip surgery (for example after total hip replacement). Please note that a femoral nerve block alone will not provide complete analgesia of the hip due to contributions from the subcostal, iliohypogastric, lateral femoral cutaneous, sciatic and obturator nerves. Therefore it is not commonly used in these cases.
Anaesthesia
- Femoral nerve block alone: skin graft or muscle biopsy from the anterior aspect of the thigh.
- In combination with sciatic and obturator nerve blocks: knee surgery
- In combination with a sciatic/popliteal block: any procedure on the lower leg or foot.
CONTRAINDICATIONS
Absolute
- Patient refusal.
- Inflammation or infection over injection site.
- Allergy to local anaesthetics.
Relative
- Anticoagulation or bleeding disorders.
- The presence of a prosthetic femoral artery graft.
- Where dense sensory block could mask compartment syndrome (for example fractures of the tibia or fibula). If unsure discuss with the surgeons prior to performing the block.
- Pre-existing peripheral neuropathies.
GENERAL PREPARATION
Before starting ensure there are appropriate indications for a femoral nerve block and no contraindications. Consent the patient and advise them on the likely duration of block. Emphasise that assistance will be required to mobilise (due to quadriceps muscle weakness) until the block has completely worn off.
Ensure the site/side is clearly marked, the patient is monitored and cannulated and that appropriate, assistance, equipment and resuscitation drugs are available. For complete details on preparation for peripheral nerve blocks please see ATOTW tutorial no.134 “Peripheral nerve blocks – Getting started”.
Specific equipment required
- 22-gauge 5cm long, short-bevelled insulated stimulating regional block needle.
- Skin antiseptic solution.
- Sterile gloves, marking pen and surface electrode.
- Peripheral nerve stimulator.
- 1-2 ml of 1% lignocaine for skin infiltration in awake patients.
- 20 ml of long-acting local anaesthetic, e.g. 0.25-0.5% Bupivacaine, Levobupivacaine or 0.2- 0.75% Ropivacaine.
PROCEDURE
Where possible the block should be performed on awake or lightly sedated patients3. This is because intra-neural needle placement may be detected earlier if the patient complains of pain on injection. In addition early symptoms of local anaesthetic toxicity such as tinnitus and confusion can be detected in awake patients. However, if spinal anaesthesia is also required this is usually performed first.
Landmarks
- Place the patient supine with leg extended.
- Identify the inguinal ligament by drawing a line between the anterior superior iliac spine and the pubic symphysis. The femoral nerve passes through the centre of this line and is at its most superficial at the level of the inguinal crease.
- Palpate and mark the femoral pulse at the inguinal ligament.
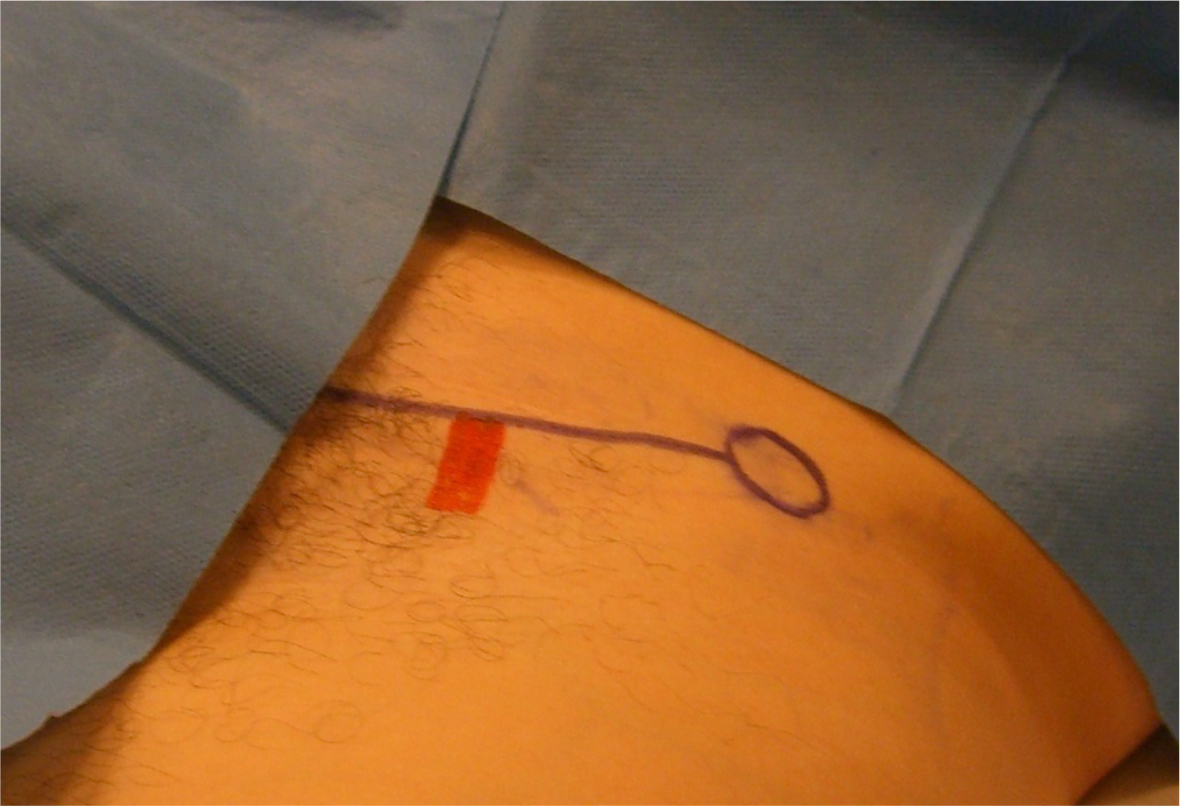
Figure 3. The inguinal ligament (black line) and the femoral pulse (red line) have been marked.
Performance of block
- The operator should stand on the side that is to be blocked, facing the patient.
- Clean the skin with antiseptic solution.
- Use 1-2mls of 1% lignocaine to anaesthetise the skin in awake patients.
- Attach the positive electrode of the nerve stimulator to the patient and the negative electrode to the needle.
- Ensure the pulse frequency of the nerve stimulator is set to 2Hz, and the pulse width to 100µs. A longer pulse width may be required in diabetic patients. If performing the block on an awake patient with a fracture it may be better to use a pulse frequency of 1Hz. Initially set the current output of the nerve stimulator to 1 or 2mA. For full details on the use of nerve stimulators for peripheral nerve blocks please see ATOTW tutorial no.149 “Nerve stimulation for peripheral nerve blockade”.
- Prepare a syringe of local anaesthetic, attach it to the needle and flush.
- Use sterile gloves and maintain a ‘no-touch’ technique.
- Needle entry point should be 1-1.5cm lateral to the artery at the midpoint of the inguinal ligament. It is recommended to palpate the femoral artery with the non-needling hand throughout the block. Stay close to the inguinal ligament, usually 1-2cm distal, as the nerve divides soon after this.
- Insert the needle through the skin and ensure that a circuit between the patient and the nerve stimulator has been completed. Most nerve stimulators have an audible beep or flashing light to indicate this.
- Direct the needle cephalad toward the centre of the inguinal ligament line at an angle of approximately 30 º to 45º.
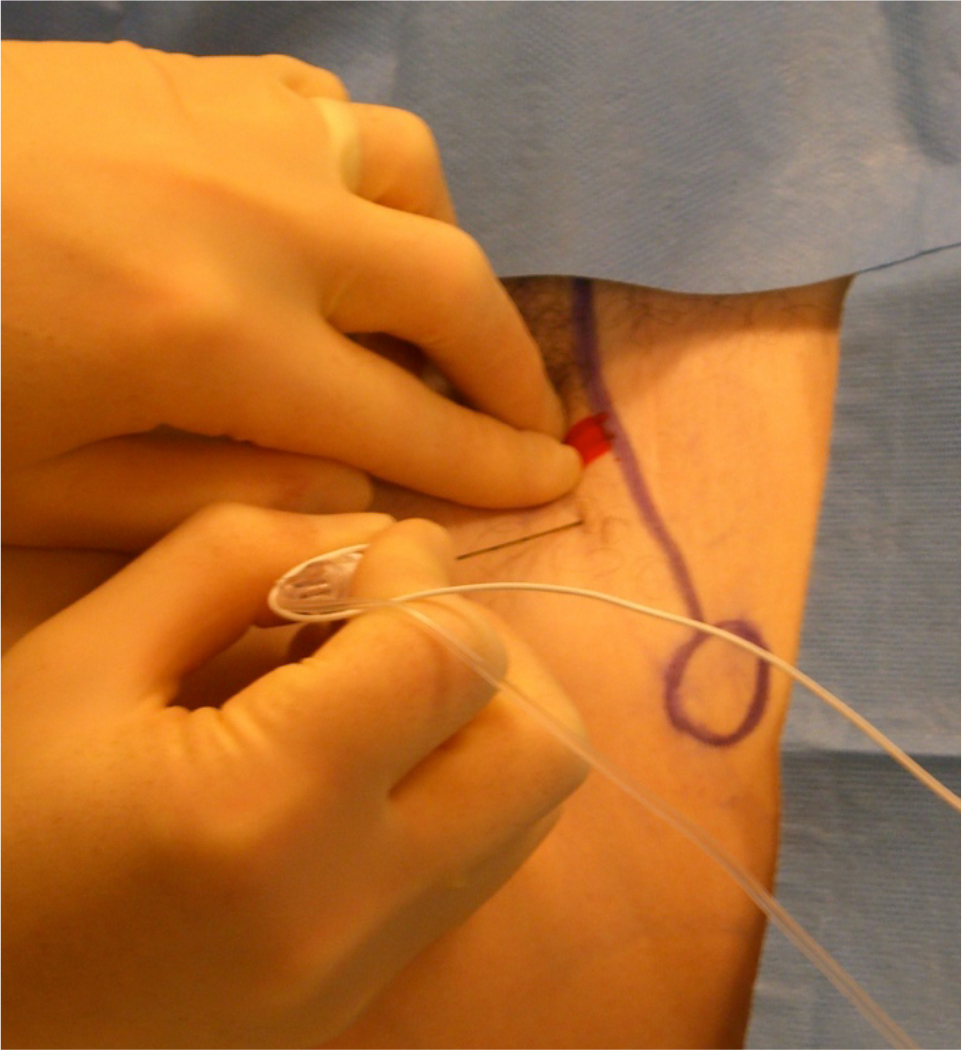
Figure 4. Needle entry is 1-1.5cm lateral to the artery and 1-2cm distal to the inguinal ligament. Aim cephalad toward the centre of the inguinal ligament line at an angle of approximately 30 º to 45º.
- The nerve is reasonably superficial at this point and is rarely deeper than 3-4cm from the skin. Two distinct ‘pops’ maybe felt as the fascia lata and fascia ilaca are crossed.
- Continue to slowly advance the needle until a motor response is obtained. The classical endpoint is the ‘dancing patella’ or ‘patella snap’ i.e. quadriceps contraction. If a motor response is not obtained and a depth of 4cm has been reached, follow the ‘needle reinsertion technique’ described in the ‘Troubleshooting’ section.
- A threshold current of between 0.2 to 0.5mA is ideal. Threshold currents below 0.2mA may indicate intraneural placement, and the needle should be withdrawn before injection. Thresholds above 0.5mA obtain low success rates.
- Once the nerve has been located satisfactorily aspirate the syringe to exclude intravascular placement.
- Inject 1ml of local anaesthetic and observe the cessation of motor twitches. If the motor twitches to not disappear, if there is high injection pressure and/or if there is any pain on injection consider intraneural needle placement and readjust the needle position.
- Inject the remainder of the local anaesthetic, aspirating after every 5mls. A dose of 20mls is usually sufficient.
Clinical tips
- When anaesthetising the skin with lignocaine, follow a line laterally to allow for more lateral needle insertion points.
- In obese patients retraction of the abdomen may be necessary to facilitate palpation of the femoral artery and performance of the block. This is best achieved with an assistant standing on the opposite of the patient to the operator and retracting with both hands. The first motor response obtained is often contraction of the sartorius muscle. This indicates stimulation of the anterior branch of the femoral nerve and the needle should be advanced deeper until contraction of the quadriceps muscle is obtained (‘patella snap’). If quadriceps stimulation is still not elicited, withdraw the needle to the skin and reinsert slightly more laterally. The posterior branch of the femoral nerve is usually lateral and deep to the anterior branch.
- After popping through the fascia iliaca, stimulation of the femoral nerve and quadriceps muscle contraction can occur suddenly and disrupt needle position. Ask your assistant to quickly turn down the stimulation current if this occurs.
TROUBLESHOOTING
Needle reinsertion technique
- If quadriceps muscle stimulation is not obtained following a needle pass, ensure a circuit has been completed between needle and nerve stimulator and recheck your landmarks. Then withdraw the needle to the skin and redirect 10-15º laterally.
- If the correct response is still not obtained, withdraw the needle completely, reinsert 1cm lateral to the previous puncture point and repeat the needle advancement.
- If necessary repeat these steps, using progressively more lateral insertion points, until the correct motor response is obtained.
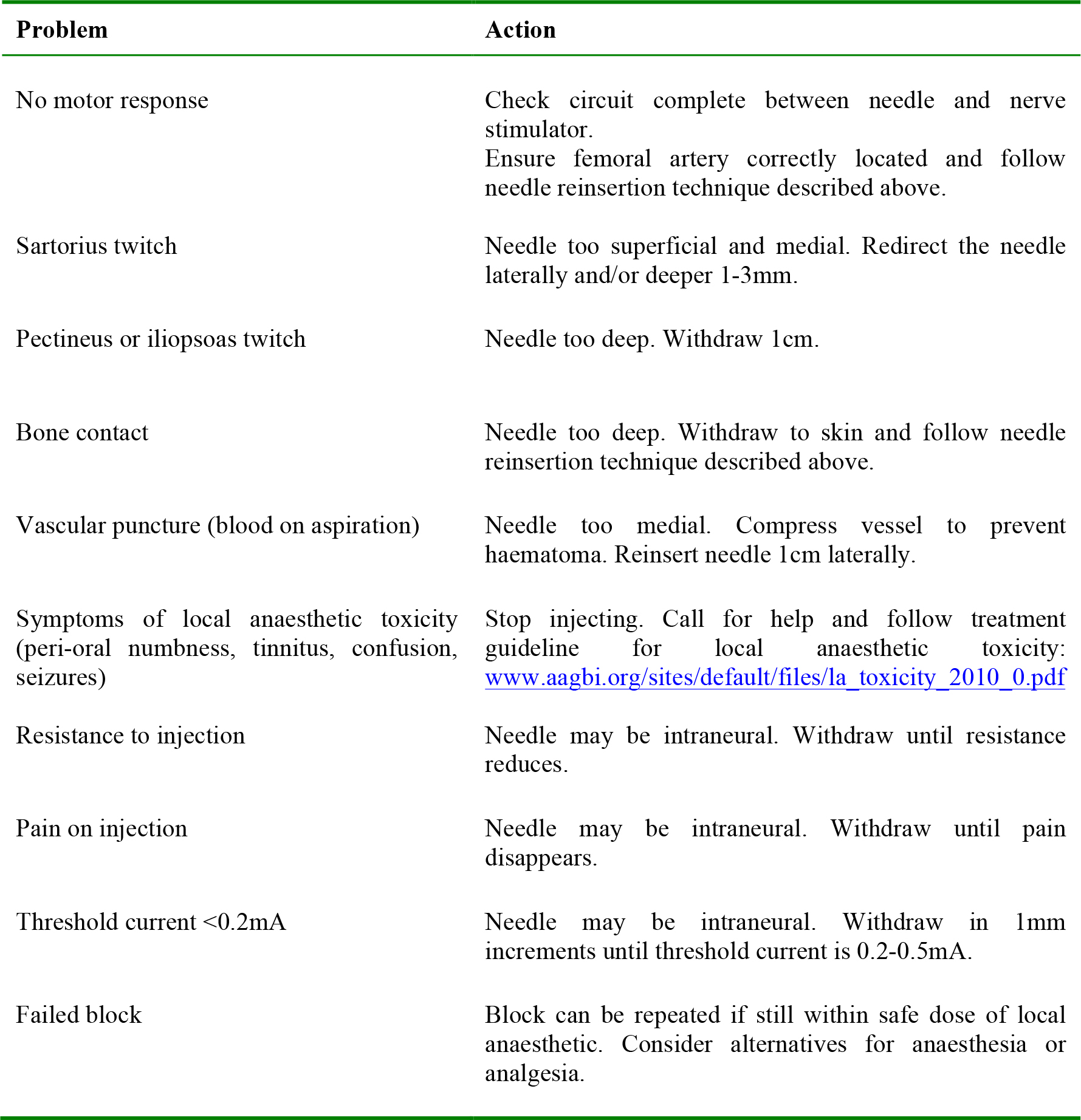
Table 1. Trouble shooting
POST-PROCEDURE CARE
- Continue monitoring the patient carefully, looking particularly for signs of local anaesthetic toxicity.
- If surgical anaesthesia is required allow time for the local anaesthetic to take effect. This will take at least 30-60 minutes. Remember that higher concentration LA is required eg 0.5% Bupivacaine or 0.75% Ropivacaine. Always test the block before allowing surgery to start and have a backup plan for block failure.
- Document the block clearly including whether done awake or after GA or spinal, the side and site of injection, needle used, volume and name of local anaesthetic, stimulation threshold in mA and any associated problems (for example paraesthesia, pain or vascular puncture).
- All patients should be seen or contacted postoperatively to ensure that the block has worn off completely.
COMPLICATIONS
Common to all blocks
- Block failure.
- Intravascular injection.
- Local anaesthetic toxicity:
- Central nervous system effects cause tinnitus, peri-oral numbness, metallic tastes, confusion and seizures.
- Cardiac effects cause tachycardia, hypertension, arrhythmias and potentially cardiac arrest.
- For details on the management of local anaesthetic toxicity please see the following guideline: www.aagbi.org/sites/default/files/la_toxicity_2010_0.pdf
- Nerve damage- temporary or permanent.
- Infection.
- Allergy to local anaesthetic.
- Methaemoglobinaemia when using Prilocaine.
Specific to Femoral nerve block
- Vascular puncture.
- Haematoma.
- Difficulty weight bearing/mobilising leading to falls and injuries.
SUMMARY
Key safety points
- Always perform the block in an appropriate setting using suitable equipment with a trained assistant and resuscitation facilities to hand.
- Always prepare your patient correctly ensuring informed consent, appropriate monitoring and intravenous access.
- Always ensure you are within the safe dose of local anaesthetic.
- Never try to inject the local anaesthetic dose if blood has been aspirated, the patient complains of pain, there is resistance to injection, or the threshold current is <0.2mA.
- If symptoms of local anaesthetic toxicity develop, stop injecting, call for help and follow the AAGBI guidelines on the management of severe local anaesthetic toxicity.
- As with any peripheral nerve block be prepared for block failure and have a backup plan.
- The femoral nerve block is one of the easiest peripheral nerve blocks to perform because the landmarks are easy to identify and the nerve is usually superficial.
- As a sole technique it provides surgical anaesthesia for a very limied number of procedures.
- In combination with a sciatic nerve block it can provide surgical anaesthesia for procedures on the lower leg or foot.
- The femoral nerve block can provide perioperative analgesia for fractured neck/shaft of femur and postoperative analgesia after knee surgery.
ANSWERS TO QUESTIONS
- Please answer True or False: The femoral nerve:
a. FALSE. The femoral nerve is derived from the ventral rami of L2 to L4
b. TRUE. The femoral vessels however are only covered by a single fascial layer, namely the fascia lata
c. FALSE. The femoral nerve is outside of the femoral sheath and is separated from the femoral vessels by a fibrous layer, part of the fascia iliaca
d. FALSE. The femoral nerve emerges from the psoas muscle at its lateral border
e. TRUE. This is why it is important to perform a femoral nerve block close to the inguinal ligament to ensure that all branches are blocked - Please answer True or False: The femoral nerve block provides:
a. FALSE. Femoral nerve block provides sensory block of the skin over the medial aspect of the lower leg
b. TRUE. The sciatic nerve supplies the flexor muscles of the knee
c. FALSE. The skin over the lateral aspect of the hip joint is supplied by the lateral femoral cutaneous nerve
d. TRUE. Only skin grafting or muscle biopsy of the anterior aspect of the thigh will be covered by femoral nerve block alone
e. TRUE. However, most of the sensory supply to the lower leg is supplied by the sciatic nerve. The continuation of the femoral nerve- the saphenous nerve only supplies sensory innervation to the medial aspect of the leg down to the medial malleolus - Please answer True or False: With regard to the performance of the femoral nerve block:
a. FALSE. The needle is too medial and should be redirected laterally and deeper
b. TRUE. This is a useful landmark
c. FALSE. The obturator nerve is rarely blocked with this technique
d. TRUE. The ‘pops’ represent the fascia lata and fascia iliaca
e. FALSE. The correct motor endpoint is quadriceps contraction which causes the ‘dancing patella’ or ‘patella snap’
WEBLINKS
- www.nysora.com/peripheral_nerve_blocks/nerve_stimulator_techniques/3100-femoral-nerveblock.html
- www.raeducation.com/blocks/lower-extremity-nerve-blocks/femoral-nerve-block/
- www.regionalworks.ca/femoral_t.html
- www.nerveblocks.net/tutorium/?lang=en_EN&main=3&sub=2§ion=content
- www.aagbi.org/sites/default/files/la_toxicity_2010_0.pdf
- www.lipidrescue.org/
REFERENCES and FURTHER READING
- Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d’Athis F. Comparison of the Three-in-One and Fascia lliaca Compartment Blocks in Adults: Clinical and Radiographic Analysis. Anesth Analg1998; 86:1039-44
- Lang SA, Yip RW, Chang PC. The femoral 3-in-1 block revisited. J Clin Anesth 1993; 5:292-296
- Ridgway S, Herrick M. Perioperative nerve dysfunction and peripheral nerve blockade. Contin Educ Anaesth Crit Care Pain (2006) 6 (2): 71-74.
- Murray JM, Derbyshire S, Shields MO. Lower limb blocks. Anaesthesia, 2010; 65 (Suppl. 1): 5766 Femoral nerve blockade.
- Vloka JD, Hadzic A, Drobnik L, Ernest A, Reiss W, Thys DM: Anatomical landmarks for femoral nerve block: a comparison of four needle insertion sites. Anesth Analg 1999; 89:1467-70
- Wang H, Boctor B, Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med. 2002; 27:139-44
- Nicholls B, Conn D, Roberts A. The Abbott Pocket guide to Practical peripheral nerve blockade Maidenhead, Abbott Laboratories Ltd 2003
- Drake et al. Gray’s Anatomy for Students 1st edition
- Association of Anaesthetists Great Britain & Ireland (AAGBI) 2002 Infection Control in Anaesthesia London, AAGBI
- Association of Anaesthetists Great Britain & Ireland (AAGBI) 2007a Standards of Monitoring During Anaesthesia and Recovery 4th Edition London, AAGBI
- Association of Anaesthetists Great Britain & Ireland (AAGBI) 2007b Guidelines for the Management of Severe Local Anaesthetic Toxicity London, AAGBI
Sources of Images:
Fig 1: Gray’s Anatomy of the Human Body www.en.wikipedia.org/wiki/File:Gray822.png
Fig 2: Gray’s Anatomy of the Human Body www.en.wikipedia.org/wiki/File:Gray546.png
Fig 3, 4: A. McEwen’s personal archive



