Basic Sciences
QUESTIONS
Before reading this tutorial try and answer the following questions. The answers with brief explanations can be found at the end of this article.
- Regarding cardiotocography (CTG):
a. Three transducers are typically used
b. One transducer is routinely placed on the fetal scalp
c. It only records fetal heart rate
d. It will detect all cases of fetal distress
e. Loss of contact is a common problem with the transducers - The following are indications for CTG monitoring during labour:
a. Primigravida deliveries
b. Women receiving epidural analgesia
c. Women with a previous caesarean section
d. Maternal pyrexia
e. Augmentation of labour with syntocinon (oxytocin) - Regarding characteristics of CTG:
a. The normal fetal heart rate baseline is 110 – 160 beats per minute
b. Variability of the fetal heart rate is a normal phenomenon
c. All decelerations are pathological
d. Most accelerations are pathological
e. Bradycardia is defined as a fetal heart rate <80 beats per minute - Regarding fetal distress:
a. It may be identified by fetal bradycardias or fetal heart accelerations
b. It may recover without intervention
c. If suspected, an emergency caesarean section must always be performed
d. It is only caused by fetal problems or abnormalities
e. Changing maternal position may be beneficial
INTRODUCTION
Continuous electronic fetal monitoring is commonly performed by cardiotocography (CTG). The CTG monitor records both fetal heart rate (cardio) and maternal uterine contractions (toco). An understanding of the principles of CTG monitoring and a systematic approach to CTG analysis may enable anaesthetists to better appreciate why obstetricians make specific clinical decisions. This understanding may aid communication and timely delivery especially when the fetus is considered at high risk.
CARDIOTOCOGRAPHY
The CTG monitor records the fetal heart rate (FHR) either from a transducer placed on the woman’s abdomen or an electrode placed on the fetal scalp. An additional transducer placed on the woman’s abdomen simultaneously records uterine muscle contraction. These variables are plotted graphically so that variations in FHR can be viewed over time and interpreted in the context of the contractile state of the uterus (Fig. 1).
INDICATIONS FOR CONTINUOUS CTG MONITORING
Intermittent auscultation of the FHR is recommended for women considered at low risk of complications during labour. The UK National Institute of Health and Clinical Excellence (NICE) make recommendations for continuous CTG monitoring which include:1
- Meconium staining of liquor
- Maternal pyrexia – defined as 38.0 °C or 37.5 °C on two occasions two hours apart
- The use of oxytocin for labour augmentation
- Fresh bleeding developing in labour
- At the woman’s request
- Abnormal FHR detected during intermittent auscultation:
• FHR <110 beats per minute (bpm)
• FHR >160 bpm
• Any decelerations after a contraction - Women receiving regional anaesthesia/analgesia. Continuous electronic fetal monitoring is recommended for at least 30 minutes during establishment of regional analgesia and after administration of a further bolus of local anaesthetic agent. In most UK centres, continuous CTG monitoring is performed after the insertion of a labour epidural.
CHARACTERISTICS OF THE CTG
A combination of several abnormalities increases the likelihood of fetal distress. Suspicious or abnormal features include:
- Baseline FHR outside normal range of 110 – 160 bpm
- Baseline variability <5 bpm
- Reduced or absent accelerations
- Presence of decelerations
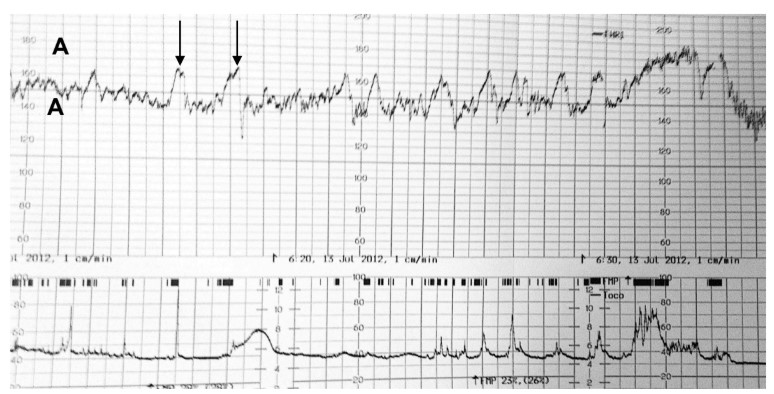
Figure 1. Normal CTG with fetal heart rate upper (A) and the tocogram, showing uterine contractions lower (B). The fetal heart rate is within the normal range and has normal baseline variability. The arrows demonstrate healthy fetal heart rate accelerations
Baseline rate
The normal baseline fetal heart rate is defined as 110 – 160 bpm. Fetal bradycardia is a baseline rate of <110 bpm. Fetal tachycardia is a baseline rate of >160 bpm.
Many fetal baseline bradycardias have no identifiable cause but may occur as a result of:
- Cord compression and acute fetal hypoxia
- Post-maturity (> 40 weeks gestation)
- Congenital heart abnormality
Fetal tachycardia is associated with:
- Excessive fetal movement or uterine stimulation
- Maternal stress or anxiety
- Maternal pyrexia
- Fetal infection
- Chronic hypoxia
- Prematurity (<32 weeks gestation)
Fetal heart rate variability
Variability refers to the normal beat to beat changes in FHR. Normal variability is between 5-15 bpm. Variability can be measured by analysing a one-minute portion of the CTG trace and assessing the difference between the highest and lowest rates during that period. Variability can be defined as:
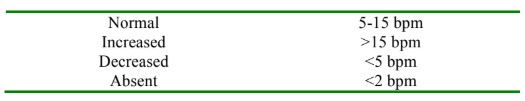
Table 1. Values for CTG Variability
Fetal hypoxia may cause absent, increased or decreased variability. Other causes of decreased variability include: normal fetal sleep-wake pattern, prematurity and following maternal administration of certain drugs including opioids.
Accelerations (Fig. 2)
Accelerations are periodic, transient increases in FHR, defined as an increase in FHR >15 bpm for more than 15 seconds When accelerations are present, the CTG is said to be reactive. Accelerations are often associated with fetal activity and are considered an indication that the fetus is healthy.
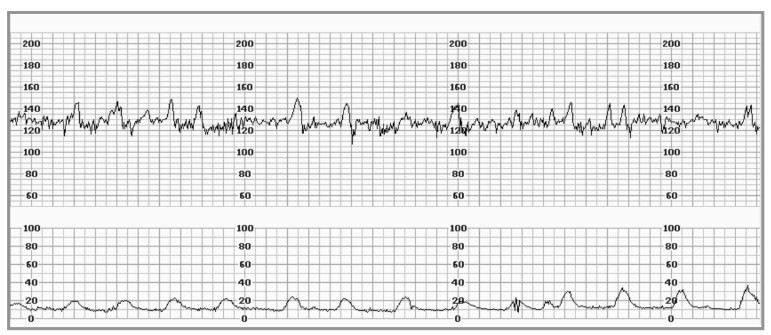
Figure 2. CTG demonstrating fetal heart rate accelerations
Decelerations
Decelerations are periodic, transient decreases in FHR, usually associated with uterine contractions. They can be subdivided into four main types by their shape and timing in relation to uterine contractions. Uterine contractions must be monitored adequately in order for a deceleration to be correctly classified.
Decelerations may be:
- Early
- Late
- Variable
- Prolonged
Early decelerations (Fig. 3)
Early decelerations tend to occur with each contraction and are uniform in shape. Early FHR decelerations appear as a mirror image of the uterine contraction trace. The onset of the deceleration occurs at the onset of the contraction and the baseline FHR recovers by the end of the contraction. The FHR usually does not fall by more than 40 bpm during an early deceleration.
Early decelerations are caused by compression of the fetal head during a contraction. They are often relieved by changing maternal posture and are a normal finding in the second stage of labour. They are not associated with a poor fetal outcome.
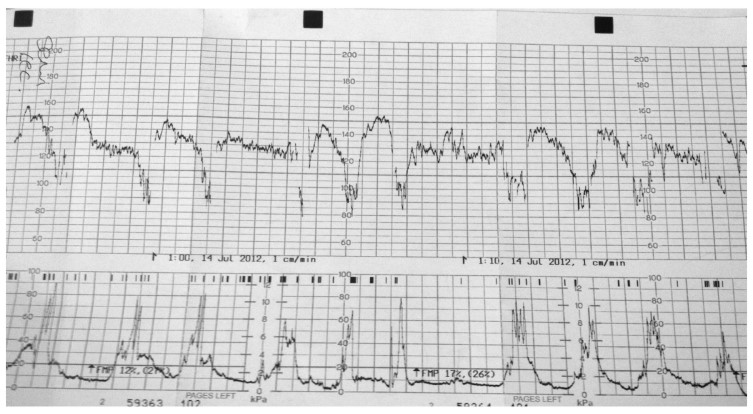
Figure 3. CTG demonstrating early decelerations. Note the onset of the deceleration occurs with the onset of the uterine contraction
Late decelerations (Fig. 4)
Late decelerations are uniform in shape on the CTG, but unlike early decelerations start after the peak of the uterine contraction. A deceleration in which the lowest point occurs more than 15 seconds after the peak of the uterine contraction is defined as a late deceleration. They are often associated with a decrease in the variability of the baseline FHR.
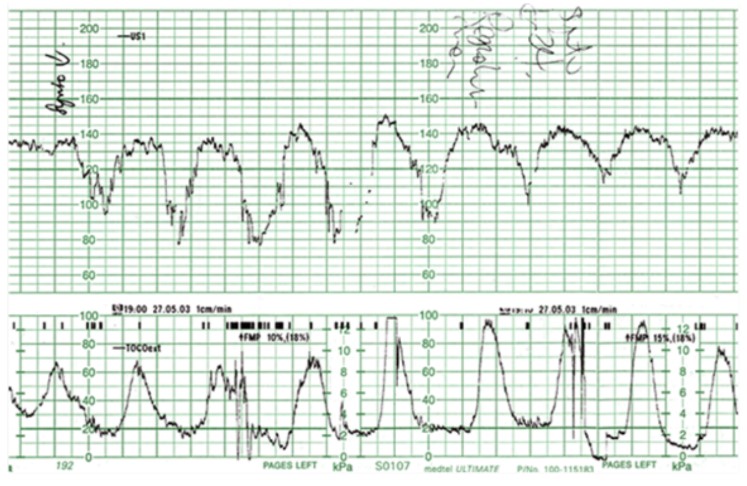
Figure 4. CTG demonstrating late decelerations resulting from cord compression
Late decelerations are associated with decreased uterine blood flow and can occur as a result of:
- Hypoxia
- Placental abruption
- Cord compression / prolapse
- Excessive uterine activity
- Maternal hypotension / hypovolaemia
Variable decelerations (Fig. 5)
Variable decelerations describe FHR decelerations that are both variable in timing and size. They may be accompanied by increased variability of the FHR. They are caused by compression of the umbilical cord and may reflect fetal hypoxia.
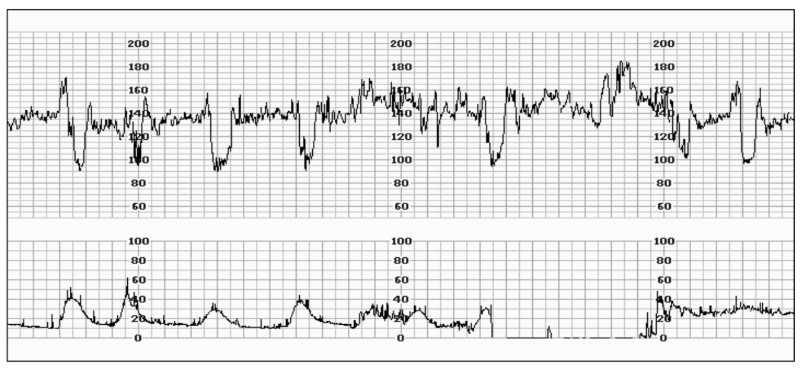
Figure 5. CTG demonstrating variable decelerations
Prolonged decelerations/ bradycardia (Fig. 6).
A deceleration with a reduction in FHR of greater than 30 bpm that lasts for at least 2 minutes is termed a prolonged deceleration They are caused by a decrease in oxygen transfer to the fetus so can arise as a consequence of a wide variety of disorders including:
- Maternal hypotension
- Umbilical cord compression
- Uterine hypertonia
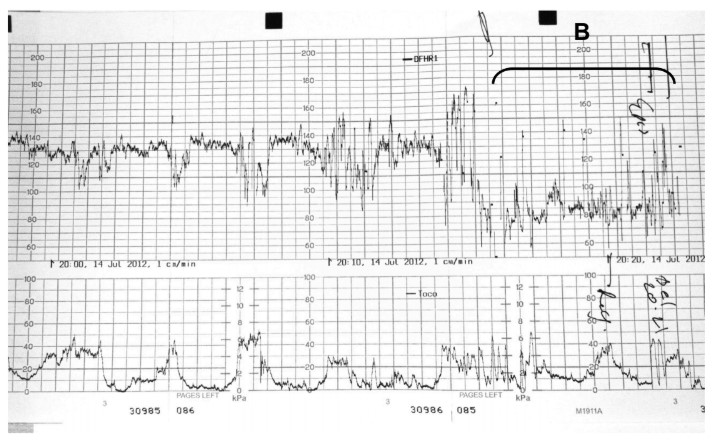
Figure 6. Prolonged deceleration/bradycardia (A – bracketed) representing fetal distress
CTG CATEGORISATION
Following CTG analysis, the findings can be used to categorise the CTG as: normal, suspicious or pathological. Many UK maternity units have adapted recommendations from NICE to produce a sticker (fig. 7 below) that is placed in the records of the labouring woman to assist her on-going management.
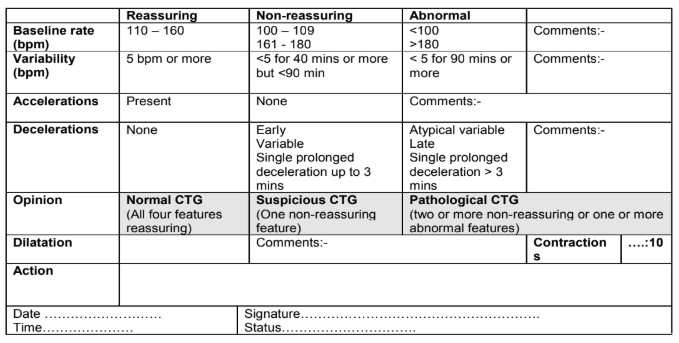
Figure 7. Sticker for maternal notes to assist with CTG guided management
FETAL SCALP ELECTRODE
A fetal scalp electrode is a device that is attached to the skin of the presenting part (most commonly the scalp) to assess fetal heart rate pattern when external monitoring cannot be used or when the quality of external monitoring is poor (e.g. maternal obesity). It provides a more accurate and consistent transmission of the fetal heart rate than external monitoring because external factors such as movement do not affect it.
FETAL BLOOD SAMPLING
Fetal blood sampling (FBS) involves taking a small sample of blood from the presenting part of the fetus during labour. FBS is advised in the presence of a pathological CTG unless there is clear evidence of severe fetal compromise. If fetal compromise is evident, (e.g. prolonged deceleration of greater than 2 minutes duration), FBS should not be undertaken and the baby should be delivered urgently. Other contraindications to FBS include:
- Maternal infection (such as HIV, hepatitis, herpes simplex virus)
- Fetal bleeding disorders
- Prematurity (<34/40)
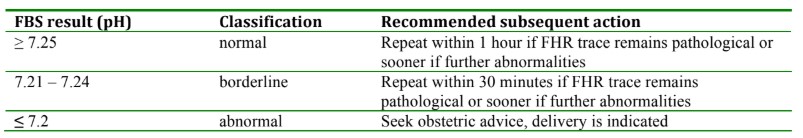
Table 2. Classification of fetal blood sampling (FBS) results1
INTRAUTERINE FETAL RESUSCITATION
If CTG monitoring indicates serious fetal compromise, or FBS result is abnormal, a decision to deliver, often by emergency caesarean section, should be made. A number of manoeuvres can be performed to improve fetal oxygenation before delivery.2 These may be performed with continuous CTG monitoring and if successful may reduce the urgency to deliver allowing time to provide neuraxial anaesthesia. These can be remembered by the mnemonic SPOILT:
- Syntocinon off
- Position full left lateral
- Oxygen
- I.V. – infusion of crystalloid fluid
- Low blood pressure – if present give i.v. vasopressor
- Tocolysis – terbutaline 250 mcg sc (a β2-agonist) or GTN (2 x 400mcg puffs sublingual)
REFERENCES
- Guideline CG55, National Institute for Health and Clinical Excellence, September 2007. Intrapartum care: management and delivery of care to women in labour. Available at: http://guidance.nice.org.uk/CG55
- Thurlow JA, Kinsella SM. Intrauterine resuscitation: active management of fetal distress. Int J Obstet Anesth 2002; 11: 105-16
ANSWERS TO MCQS
- a. F
b. F
c. F
d. F
e. T
The CTG monitor typically has 2 transducers that are placed on the abdominal wall unless monitoring a woman with multiple pregnancy. It is non-invasive and carries no direct risk of harm to the fetus. One transducer records the fetal heart rate and the second records maternal uterine contractions. Loss of contact between transducer and the abdominal wall is a common problem. Lubricating jelly is used to help prevent this. Continuous CTG monitoring may restrict the woman’s movement and in some positions (e.g. during insertion of an epidural) accurate fetal heart rate monitoring may be difficult. - a. F
b. T
c. T
d. T
e. T
Indications for continuous CTG monitoring are outlined by NICE1.For low risk deliveries, the fetal heart rate should be checked every 15 minutes during the first stage of labour, increasing to every 5 minutes during the second stage. Continuous monitoring is recommended for higher risk pregnancies, including: previous caesarean section, induction of labour, pre-eclampsia, maternal diabetes, breech deliveries and multiple pregnancies. - a. T
b. T
c. F
d. F
e. F
The normal baseline fetal heart rate is 110 – 160 bpm. A heart rate of less than 110 is defined as a fetal bradycardia. Fetal heart rate variability is a normal feature and should be in the region of 5 – 15 bpm. Accelerations are viewed as a normal and reassuring feature and some but not all decelerations are concerning. - a. F
b. T
c. F
d. F
e. T
Fetal distress is indicated by fetal bradycardia or variable/late decelerations. It may recover spontaneously or with simple measures such as moving the woman into the left lateral position. As well as fetal problems, it can be precipitated by maternal problems including hypotension.



