Basic Sciences
KEY POINTS
- Humidity describes the amount of water vapour within a gas
- Multiple devices are available to measure the humidity of gases
- Failure to humidify gases can cause patient complications
- Humidification is vital for a safe and comfortable theatre environment
- Devices for inspired gas humidification are either active of passive
INTRODUCTION
Substances exist as solids, liquids or gases. In the liquid phase molecules move randomly and have a variable kinetic energy. At the surface of a liquid some molecules can escape the intermolecular forces keeping them in liquid form and evaporate to form a vapour. The molecules which escape are the ones with the highest kinetic energy, therefore the average kinetic energy of the remaining liquid and therefore its temperature falls1.
If the liquid is left within a sealed container equilibrium is reached between molecules leaving and re-entering the liquid. The vapour above the liquid will saturate the gas and exert a partial pressure. At equilibrium this is known as the saturated vapour pressure1. If heat energy is added to the system the kinetic energy of the molecules increases, therefore the amount of substance escaping the liquid state increases. This in turn raises the saturated vapour pressure. The amount of heat energy required to turn 1g of substance from liquid to vapour at a given temperature is the latent heat of vaporisation1. If heat is not added to the system the energy is obtained from within the liquid and it cools. This is the reason for temperature compensation in anaesthetic vaporisers.
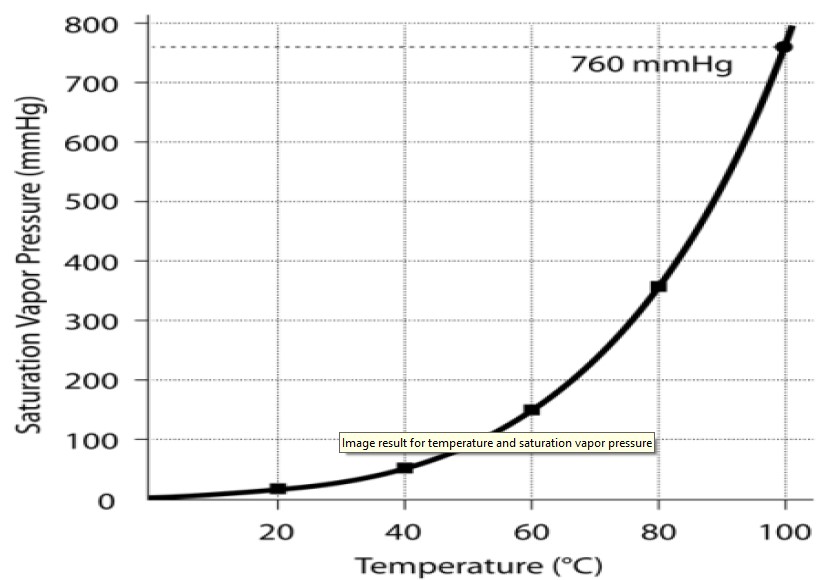
Fig 1. The effect of temperature on SVP
Humidification describes the addition of water vapour to a gas. Absolute humidity is the amount of water vapour within a gas and is measured in g.m-3 or or mg/L. The relative humidity is a ratio of amount of measured water vapour in a gas divided by the saturated vapour pressure at a given temperature1,2. As the temperature of a gas increases the amount of water vapour it can hold and therefore its saturated vapour pressure increases (table 1/fig 1).
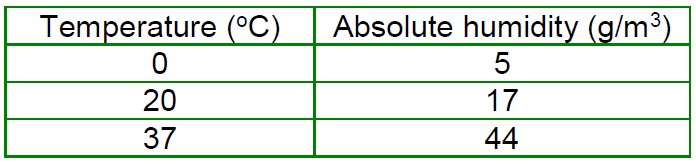
Table 1. The effect of temperature on absolute humidity1
Lowering the temperature of a gas decreases the amount of water vapour it can hold. The temperature at which a mass of air is at 100% relative humidity is the dew point. At the dew point water vapour condenses into the liquid water at the same rate at which it evaporates. If the dew point is below 0°C it is known as the frost point1.
Humidity and anaesthesia
Indoor air at 20°C has a relative humidity of 50-60%3. As this air passes through the nasopharynx it is heated and fully saturated to an absolute humidity of 44g/m3 (figure 1). The point of full saturation during normal respiration is the isothermic saturation boundary and is just above the carina2. The nose is well adapted for increasing relative humidity as it is a highly vascular area and the presence of nasal turbinates increases the surface area for heating and humidification.
Airway epithelial cells secrete mucus; this lubricates the airways and provides a medium for trapping inhaled particles and pathogens. Mucous is moved toward the nasophaynx by the rhythmic beating of cilia and debris is cleared. Bypassing the nasopharynx with either an endotracheal or tracheostomy tube delivers cold dry gas to the airway. The air is humidified by evaporation of liquid from this mucus layer. This causes drying of mucus, and heat loss due to the latent heat of vaporisation. Loss of heat through this mechanism is of importance in paediatric practice. Children, especially neonates have a high minute volume to body surface area ratio and ventilation for 90 minutes with un-humidified air can lead to a fall in body temperature of 0.75 °C3.
Inadequate humidification of the airway leads to thick tenacious sputum. This is difficult to clear and can lead to mucus plugs that may block endotracheal tubes and even airways. This may expose patients to distal atelectasis, V/Q mismatching and increased risk of infection. As exposure time increases, so does the damage. Prolonged exposure to unhumidified gases can lead to loss of cilia number and function, airway keratinization and airway necrosis3,4. During ventilation in critical care, these complications can lead to increased incidence of ventilation associated pneumonia, increased work of breathing and prolonged ventilator time/ difficulty weaning from mechanical ventilation.
Humidity also plays a role in the operating theatre. If the relative humidity is too high, it becomes uncomfortable for staff as heat loss through sweating is reduced. If humidity is too low, there is an increased risk of fire and explosions. Low humidity has also been associated with worsening of rhinitis and asthma. A balance is reached at a humidity of 50-60%4.
Measurement of atmospheric humidity
Anything that measures humidity is known as a hygrometer. Devices that measure humidity can be divided into those which measure relative humidity such as the hair hygrometer, wet and dry bulb hygrometer, Regnaults hygrometer, and those which measure absolute humidity such as transducers and mass spectrometry.
Hair Hygrometer
Human and different types of animal hair have been used in the hair hygrometer. It works on the principal that as humidity increases the length of a hair increases. The hair is tensioned so that the end remains fixed while the other is free to expand over a pre-calibrated scale. The hair hygrometer is accurate between 30-90 % relative humidity5.
Wet and dry bulb hygrometer
Two mercury thermometers are used. The dry bulb is in equilibrium with the ambient air temperature. The wet bulb is suspended in water. The wet bulb is cooled by the latent heat of vaporisation as the water evaporates. The rate of evaporation is proportional to the relative humidity above the water. Higher humidity causes less water to evaporate and there is less cooling of the wet bulb. The temperature difference between the two bulbs can be referenced using set tables and relative humidity calculated. To ensure accuracy, a constant airflow is required over the device to prevent build up of humidity1.
Regnaults hygrometer
Air is passed through a silver tube containing ether which causes the air to cool. Once the air reaches its dew point (100% relative humidity), condensation occurs on the outside of the tube. Relative humidity can be calculated from the temperature of the dew point by using set tables. This is the most accurate measurement of relative humidity5.
Absolute humidity
Absolute humidity can be measured by a mass spectrometer and transducers. Transducers work on the principle that electrical resistance or capacitance changes with increasing humidity. Mass spectrometers measure breath by breath humidity in gas samples but require no condensation in the sample line1.
Methods of upper airway humidification
The ideal humidification device is one which:
- Is cheap
- Is simple to use
- Does not increase risk of infection
- Humidifies and heats gases to physiological conditions
- Does not produce significant resistance to breathing or increases dead space
The sizes of water droplets provided by humidification devices are of importance. The ideal size is 1 micron, this is transferred to the alveoli. Larger droplets of 5 microns deposit in the trachea and have no benefit for the distal airways. Droplets of 20 microns and above are responsible for the condensation seen of ventilation tubing5. Current devices can be classified as active and passive systems. Passive systems do not rely on external power or water, active systems do.
Heat and Moisture exchangers
The most commonly used passive humidifiers is the heat and moisture exchanger (HME). A HME consists of a membrane (commonly paper, ceramic or polyurethane foam) coated in a hygroscopic material (calcium or lithium chloride) suspended in a lightweight plastic casing with an inlet and an outlet1. Warm humidified gas is expired and condenses on the membrane. As cold dry gas is inspired it passes over the filter and becomes humidified and warmed. It takes 20 minutes to reach maximum efficacy producing a relative humidity of 70%1,5.
Advantages – Simple and cheap to use. Can incorporate a micro bacterial filter (HMEF) (Figure 2).
Disadvantages– bulky and needs to be close to the patient to minimise dead space. Less efficient at high minute volumes and can become blocked with secretions and so significantly increase airway resistance. It needs replacing every 24 hours.
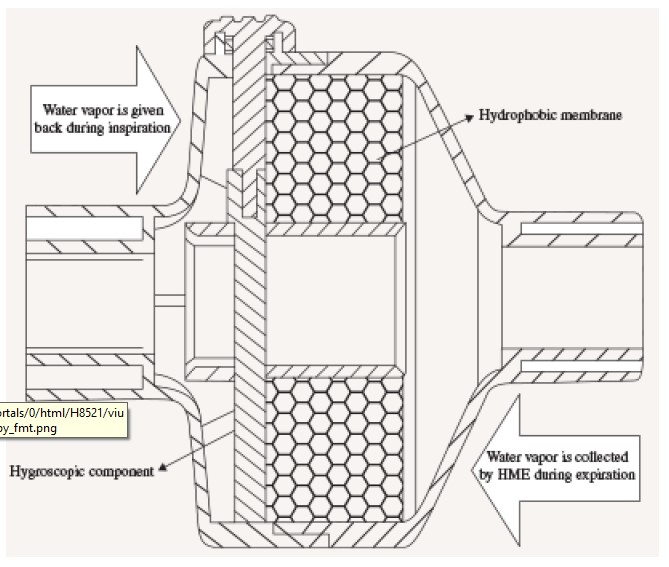
Figure 2. Schematic diagram of HME filter
Active Humidifiers
Water bath humidifiers
Gases can be bubbled through water to increase humidity. Passing gas through water at room temperature causes the gas to cool due to latent heat of vaporisation. The water bath can be heated. This improves the efficiency of the device and also reduces the incidence of bacterial colonisation.
Advantages – High relative humidity can be achieved. Warms inspired gases.
Disadvantages – Bacterial contamination if not heated to 60°c. Risk of aspiration of water into the airways. Risk of airway burns with high temperatures.
Nebulisers
Nebulisers use a venturi system which employs the Bernoulli effect. A gas at high flow passes through a constriction causing the gas to accelerate, reducing its potential energy allowing other gases or liquids to be entrained. This can include medications or in the case of humidification, water vapour. The size of the water droplet produced by nebulisation determines where in the airway it is deposited2. Standard nebulisers produced droplets of 4 microns in diameter and these are deposited in the upper airway and trachea. Efficacy can be improved by passing the droplets over an anvil which further reduces particle size. The most efficient form of nebuliser is the ultrasonic nebuliser. Here a transducer immersed in water and vibrated at a frequency of 3MHz produces1-2micron droplets. These particles easily reach the bronchioles and provide excellent humidification.
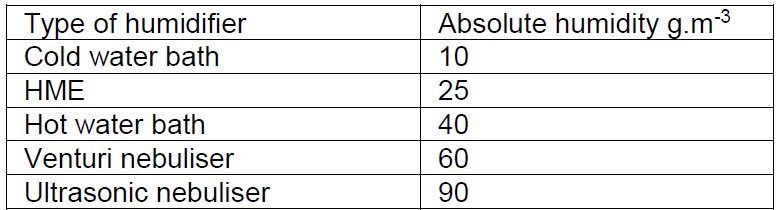
Table 2- Efficacy of different humidification device6
SUMMARY
- As air passes through the nasopharynx, it is heated and humidified to an absolute humidity of 44g/m3
- Invasive airways bypass protective airway mechanisms to pathogens and particles
- Prolonged exposure to un-humidified gases may lead to cilia dysfunction and airway injury
- Hygrometers are devices that measure humidity, either absolute or relative humidity
- The most commonly used passive humidifiers is the heat and moisture exchanger (HME)
REFERENCES AND FURTHER READING
- Davis PD, Kenny GNC, Humidification. In: Basic physics and measurement in anaesthesia (2003). Butterworth Heinmann. Pages 127-137
- McNulty G, Eyre L. Humidification in anaesthesia and critical care. BJA education 2015; 15(3): 131-135
- Gross JL, Park GR. Humidification of inspired gases during mechanical ventilation. Minerva anaestesiol.2012; 78(4): 496-502
- Shelley MP, Lloyd GM, Park, GR. A review of mechanisms and methods of humidification of inspired gases. Intensive care med 1988; 14: 1-9
- Tidmarsh M, Lin S. Humidity measurement. In: fundamentals of anaesthesia (2008). Cambridge University press. Pages824-826.
- Shenoy S. Humidification. Update in anaesthesia.2008; 24(2): 151-15



