General Topics
Self assessment
Complete the following questions before reading this tutorial.
- A 65yr old man is listed for a total knee replacement. During your assessment for anaesthesia you notice his pre-assessment blood pressure is 190/100. What is your management?
- Which drugs are commonly used to treat hypertension both in the long term and acute situation?
- You are called to recovery to review a 77yr old patient with a blood pressure of 210/110 after a laparoscopic cholecystectomy. What is your management?
- What are the complications of long standing hypertension?
- How can blood pressure be measured?
Introduction
Hypertension is a common medical condition. The World Health Organisation classify a patient as hypertensive if a series of blood pressure recordings reveal values greater than 160/100. It is important to investigate and treat persistent hypertension for a variety of reasons. The long term end organ effects are numerous and add significantly to patient morbidity and mortality. Ensuring cardiovascular stability and pre-optimisation of blood pressure allows us to manipulate physiology and pharmacology more safely during anaesthesia.
It is necessary to understand the physiology of blood pressure control and how this is affected by anaesthesia.. The physiology of ageing is also an important component of blood pressure control as the arterial system becomes increasingly rigid secondary to arteriosclerosis..
General considerations
When assessing patients for anaesthesia who have elevated blood pressure, a number of questions must be answered.
- Is the patient known to be hypertensive on a previous occasion?
- Are they on antihypertensive medication?
- Does the patient have a treatable cause for their hypertension?
- Does the patient have “white coat” hypertension?
- Does the blood pressure control need alteration before surgery?
Untreated, severe hypertension can lead to serious post operative complications for example myocardial infarction, cerebral haemorrhage, infarction and renal failure.
Preoperative assessment
When assessing a patient for anaesthesia, ask about related illnesses such as ischaemic heart disease, renal failure and cerebrovascular disease. This can assess the extent of hypertensive end organ damage, and therefore risk for anaesthesia. Initial investigations which should be considered include electrocardiography (ECG) and electrolyte measurement. ECG changes which may include left ventricular hypertrophy, bundle branch block and evidence of old myocardial infarction such as Q waves. In breathless patients a chest radiograph should be performed, and if significant cardiac disease is suspected an exercise tolerance test.
Approximately ninety percent of patients have idiopathic (no underlying cause) hypertension, but any treatable causes such as endocrine tumours, renal disease and pregnancy related disorders such as pre-eclampsia should be excluded. Patients with uncontrolled hypertension requiring urgent surgery may benefit from regional anaesthetic techniques to avoid the risks of general anaesthesia, for example an ankle block for toe amputation.
Investigation
Patients with hypertension are often asymptomatic, and preoperative assessment with routine blood pressure measurement, is often the first manifestation of any potential problem. Blood pressure is measured according to the Korotkoff sounds which represent turbulent flow within the artery. Systolic blood pressure is measured at the first sound, and diastolic between the fourth and fifth sounds, which represents the point before absence of turbulent flow.
Incidental hypertensive findings may indicate long standing hypertensive disease. In order to determine this , a series of blood pressure measurements, taken with the correct size cuff. This is calculated by measuring the circumference of the subject’s upper arm. A suitable standard cuff between this value and 20% greater than the arm circumference is used.
Measurements should be made of a period of time to determine a consistent rise in pressure. Current guidelines suggest two subsequent measurements over a period of 2 weeks using the best conditions available. This however is not appropriate in the acute surgical setting in patients requiring urgent surgery. A number of preoperative blood pressure readings may be taken over 2 – 3 hours with the patient resting. Frequently blood pressure reduces over this time, indicating underlying anxiety as a likely cause.
Those patients with isolated “white coat” hypertension have not been shown to be at higher risk from anaesthesia than controls and therefore surgery should not be delayed unnecessarily. Elderly patients with systolic blood pressures below 180 / 190 mmHg should also be considered for surgery, particularly if there is little evidence of end organ damage, as these values are considered in the normal range for elderly patients due to normal physiological change.
Drug treatment
Pharmacological intervention can be subdivided into long term and acute therapies. Drugs used to treat hypertension act in a variety of ways. They can act locally on the vessel wall e.g. nitrates acting to increase local nitric oxide production, increase receptor activity e.g. alpha blockers reducing constriction of vessel musculature and beta blockers reducing force of contraction of cardiac muscle.
Drugs may be divided into those used for long term management of blood pressure, and those used acutely for emergency reduction of hypertension. When gaining long term control one agent will usually be started and the effect determined before starting further therapy. In the primary care setting, hypertension in the elderly is usually managed initially with a thiazide diuretic or beta blocker. ACE inhibitors are also considered in younger individuals for first line treatment. Subsequent antihypertensives may be added according to initial response.
Long term management drugs
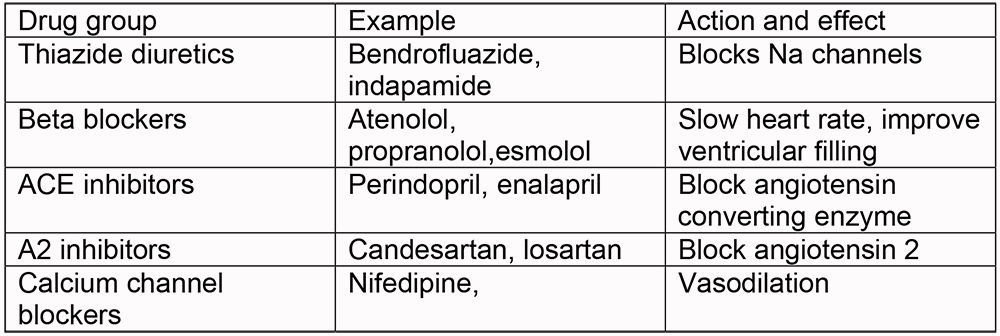
Many of the drugs used in the management of hypertension are not tolerated by patients. Diuretics act on the renal tubules and prevent reabsorption of water and solutes in the renal tubules. Complications include electrolyte disturbances, such as hypokalaemia and hyperuricaemia and patient compliance may decrease due to polyuria, particularly in the elderly and immobile. Beta blockers can precipitate lethargy, nausea and general malaise, ACE inhibitors can precipitate cough, due to reduced breakdown of bradykinin, particularly in women, and A2 inhibitors bypass this. Deterioration of renal function on commencement of ACE inhibitors prevents their use, and alternative classes of drugs must be used. This should be in the chronic drug treatment section
Conduct of anaesthesia
General principles
Cardiovascular stability is important during anaesthesia and the perioperative period. Hypertensive patients are at risk of greater swings of blood pressure than the normal population and it has been shown that blood pressure lability can be associated with increased cardiovascular morbidity and mortality postoperatively, particularly in patients with severe uncontrolled hypertension. Optimisation of such patients with investigation and drug treatment can improve long term outcome and prevent such complications.
Patients who have hypertension require a higher blood pressure for adequate organ perfusion than normotensive patients – this is particularly in the elderly. Avoidance of hypotension (and apparent normotension in patients who normally rely on higher values in everyday life), may prevent complications of under-perfusion..
Induction
Significant hypertension in the induction area often settles with a small dose of intravenous sedation (midazolam 1 – 3mg).
Persistently elevated blood pressure can prove challenging during anaesthesia. Abrupt and marked reductions in blood pressure may occur on induction of anaesthesia, and large increases during stimulating procedures such as laryngoscopy, intubation and pain. It is possible to augment induction with other pharmacological agents. Short acting opioids such as fentanyl 1mcg/kg or alfentanyl 10mcg/kg given in conjunction with induction agents will diminish stimulatory effects.
Intraoperative blood pressure monitoring may be non-invasive or invasive. Standard non-invasive blood pressure monitoring is mandatory for anaesthesia, with a minimal interval of five minutes. High risk patients undergoing major surgery can, in addition, have intra-arterial monitoring to improve control and allow early pharmacological intervention. These measures are used in conjunction with continuous monitoring of the ECG and oxygen saturation.
Maintenance
Patients with underlying organ dysfunction need careful consideration of anaesthetic agents. For example underlying renal failure, will alter metabolism and excretion of drugs. Recent or significant end organ damage, for example recent myocardial infarction may necessitate surgical delay.
Effective opioid analgesia, regional anaesthetic techniques and avoiding hypoxia, hypercarbia and light anaesthesia all aid to reduce episodes of hypertension intraoperatively. Vasopressor agents and intravenous fluids may be required if hypotension results from cardiac depression. Spinals or epidurals may increase intraoperative hypotension, particularly in hypertensive patients who are dehydrated or those receiving vasoldilator drugs..
Recovery
Monitoring should include ECG, blood pressure and SpO2. Coughing on emergence of anaesthesia may produce hypertension, and preoperative lignocaine spray on the endotracheal tube or deep extubation may improve this. Patients may develop hypertension due to pain, bladder distension or anxiety. It is also important to remember some patients will be confused and disorientated after anaesthesia and this may worsen blood pressure values. This highlights the importance of the recovery room being a suitably calm environment with staff trained to anticipate and treat these problems.
After reversible causes have been treated (pain, urine retention) treatment of continuing hypertension may be reaquired. Although there is no cut off value for treatment, a persistently elevated systolic blood pressure reaching 200mmHg would suggest treatment is appropriate.
Antihypertensive drugs and anaesthesia
Elective surgical cases are usually given their regular antihypertensive medications on the morning of surgery..
Remember that anaesthetic agents also cause vasodilation and cardiac depression, and the effects may be cumulative. Analgesic agents will reduce anaesthetic requirement and allow a smoother induction. Anaesthetic agents such as ketamine should be avoided due to their cardiovascular stimulatory properties.
Drug action and side effects
- Beta blockade has been shown in studies to improve perioperative morbidity and mortality in patients with ischaemic heart disease, although more recently meta analyses looking at atenolol have disputed this theory
- Beta blockers are avoided in patients with asthma, and may also prevent changes in the patient’s physiology to adverse events such as tachycardia which may be due to pain, reduced cardiac output, awareness, anaphylaxis or even malignant hypertension during anaesthesia. Excessive bradycardia may also cause adverse events and require treatment with anticholinergics.
- ACE inhibitors block angiotensin converting enzyme which reduces the renin angiotensin aldosterone system. ACE inhibitors will usually be continued prior to anesthesia, but cessation should be considered if marked blood loss is anticipated or regional techniques such as epidurals are carried out, as the cumulative hypotensive effects may be detrimental. Renal function should be carefully monitored in those patients taking ACE inhibitors, particularly in the perioperative period. Non steroidal anti-inflammatories should be used with caution in patients taking ACE or A2 inhibitors..
Acute management of hypertension
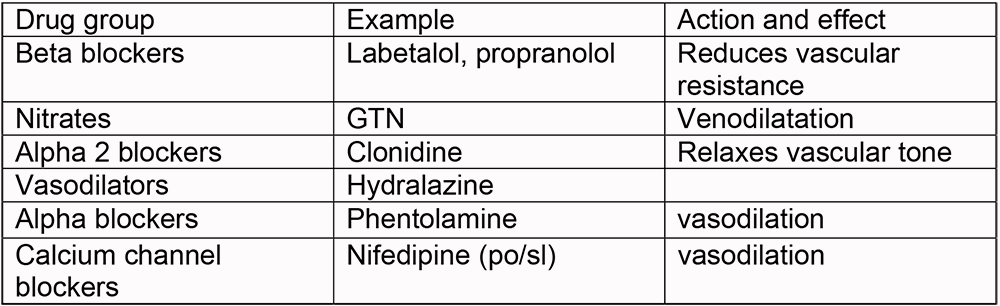
Intraoperative hypertension may have multifactorial causes, reversible causes should be excluded and anaesthesia deepened with analgesics or anaesthetic agents before using antihypertensives in the acute setting. Labetololm, a combined alpha and beta blocker with a short onset time e.g. labetalol may be titrated intravenously in patients who require supplementary treatment
Postoperative care
Patients must be followed up after anaesthesia to ensure post operative complications are minimised and treated appropriately if they occur. It is important to ensure patients continue their antihypertentsives after surgery and alternative routes of administration are considered for those patients who are nil by mouth. Patients with severe hypertension must be closely monitored and ward and anaesthetic staff alerted if management becomes difficult or is uncontrolled. High risk patients should also be given supplementary oxygen to prevent hypoxia and therefore reduce ischaemic episodes after anaesthesia. The continuation of prevention of hypertensive triggers on the ward must also be highlighted.
Further reading
- NICE guidelines for management of hypertension. Department of Health
- The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. JAMA 289(19) May 2003
Answers
- This patient initially needs standard anaesthetic assessment before anaesthesia. History of hypertension, is he on any antihypertensive drugs? Is the reading a one off value? Is there evidence of end organ damage? He needs repeat measurements in a relaxed environment and an ECG. Routine bloods should be checked. If after assessment, the hypertension is new and persists at this level, postponement of surgery and commencement of a thiazide diuretic prior to rescheduling and GP liaison would be the most sensible management of this elective case.
- See text and tables.
- This patient is severely hypertensive postoperatively. The causes of this may be multiple. Exclude pain, urinary retention, hypoxia, anxiety. Repeat blood pressure measurements regularly in addition to other routine monitoring. If hypertension persists, consider labetalol 5mg/ml and titrate to normotension for the patient concerned.
- See text regarding end organ damage and perioperative complications.
- See text



