General Topics
SELF ASSESSMENT
The aim of this tutorial is to discuss the causes and management of intraoperative hypotension. Consider the following scenario before reading the tutorial. How would you manage this case? Discuss your plan of action with your colleagues.
Case scenario
A forty-two year old female is scheduled for a laparoscopic cholecystectomy. She has a BMI of 26 and reports mild asthma for which she uses salbutamol occasionally.
Induction is uneventful. She is intubated and ventilated and remains cardiovascularly stable for the first thirty minutes of the procedure. Thereafter, her blood pressure is suddenly un-recordable, despite repositioning the cuff. On examination, she has good bilateral air entry. She is pale and cool peripherally with a weakly palpable pulse of 120.
What should you do?
What is your differential diagnosis?
What clinical signs would you expect to see for each possible cause?
Answers are given in the text.
INTRODUCTION
Severe intraoperative hypotension is an anaesthetic emergency. Swift recognition and treatment is vital to ensure adequate organ blood flow; particularly to the brain, heart, kidneys and the placenta in pregnancy. Uncorrected, ischaemic changes may ensue, with consequences including stroke, myocardial infarction, acute tubular necrosis and in obstetric patients, fetal compromise.
PHYSIOLOGY
Mean arterial pressure is a product of cardiac output and systemic vascular resistance. Cardiac output depends on heart rate and stroke volume, and therefore anything that affects these indices will impact on the blood pressure. Similarly, systemic vascular resistance depends on several factors and will vary according to the degree of sympathetic tone and the effect of vasoactive drugs, including interventions such as central neuroaxial anaesthesia
DEFINITION
The blood pressure required to maintain adequate blood flow to vital organs will vary between patients. In healthy individuals perfusion to the brain, heart and kidneys is maintained by auto-regulation at systolic pressures of 70-80 mmHg. In hypertensive patients this threshold is reduced, and in patients with atherosclerosis of the cerebral arteries, higher blood pressure may also be required to maintain flow. A reasonable approach is to aim to keep the mean arterial pressure above 75% of the patient’s normal value.
It is important to remember that blood pressure alone does not correlate with tissue perfusion, and that perfusion is more likely to be compromised where hypotension is associated with reduced cardiac output and accompanied by vasoconstriction. There may be specific signs or symptoms of inadequate organ blood flow in anaesthetised patients: ST depression an indication of poor myocardial perfusion, and nausea and dizziness often a sign of inadequate cerebral perfusion in awake patients undergoing regional anaesthesia.
RISK FACTORS
Thorough pre-operative assessment is required to identify those patients at increased risk of intraoperative hypotension so that complications can be anticipated and prevented where possible.
Co-morbidity
Patients with known hypertension are at increased risk of hypotensive episodes perioperatively, and as mentioned above are also more vulnerable to tissue ischaemia as the lower limits for autoregulation may be raised. It is therefore important to identify their usual medications and be familiar with the associated cardiovascular effects; it is common practice to omit ACE inhibitors on the day of surgery.
It is important to establish the extent of any existing myocardial disease so that the patient’s condition is optimised and pump failure is minimised perioperatively. Patients with fixed cardiac output, for example with aortic stenosis, are particularly susceptible to hypotension during anaesthesia.
There are also other systemic conditions which may predispose to intraoperative hypotension. Examples include Addison’s disease, hypothyroidism and carcinoid syndrome
In such patients where significant hypotension is anticipated it is important to minimise preoperative dehydration, insert large bore intravenous access prior to induction of anaesthesia, and consider the use of invasive blood pressure monitoring.
Hypovolaemia
A patient requiring urgent surgery may already be haemodynamically compromised due to the nature of their illness. Hypovolaemia may be due to haemorrhage, or other causes such as vomiting and diarrhoea, burns or sepsis. A thorough examination should take place to assess the degree of dehydration or shock (skin turgor, capillary refill, mucous membranes, urine output) and to replace losses preoperatively if appropriate. In a fit young person there is often no fall in blood pressure until more than 30% of the circulating volume has been lost, and blood loss is often concealed. Patients with multiple trauma in particular need thorough assessment by primary and secondary survey to establish the extent of injuries.
Anaesthetic technique
General anaesthesia commonly results in mild hypotension due to the effects of intravenous induction agents and inhalational agents in reducing cardiac output and systemic vascular resistance. In the elderly induction agents need to be given slowly and at reduced doses to avoid severe hypotension.
Spinal and epidural anaesthesia cause vasodilatation due to sympathetic block, and if the block is above T4 may also result in decreased myocardial contractility and bradycardia.
Patients undergoing combined regional and general anaesthesia are particularly susceptible to hypotension.
Pregnancy
Obstetric patients undergoing surgery are at risk of hypotension due to aorto-caval compression compromising venous return, minimised by use of left lateral tilt to displace the gravid uterus.
DIFFERENTIAL DIAGNOSIS
In the event of intraoperative hypotension, a rapid assessment of the patient is required. This should take into consideration:
- risks associated with the anaesthetic technique
- risks specific to the type of surgery or approach
- known or possible allergies
It is important to consider measurement error and repeat the reading to establish it as ‘real’. When using non- invasive blood pressure measuring it is possible to estimate the systolic pressure by palpating a distal pulse during deflation of the cuff. If using invasive monitoring it is important to check that the level of the transducer is correct.
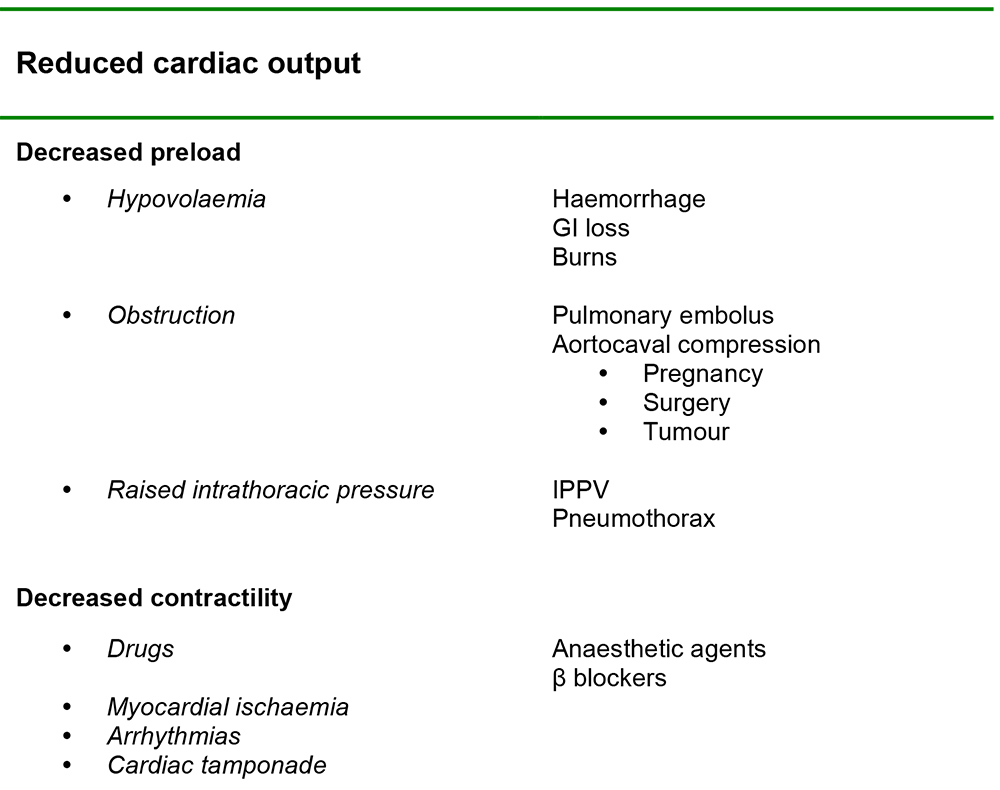
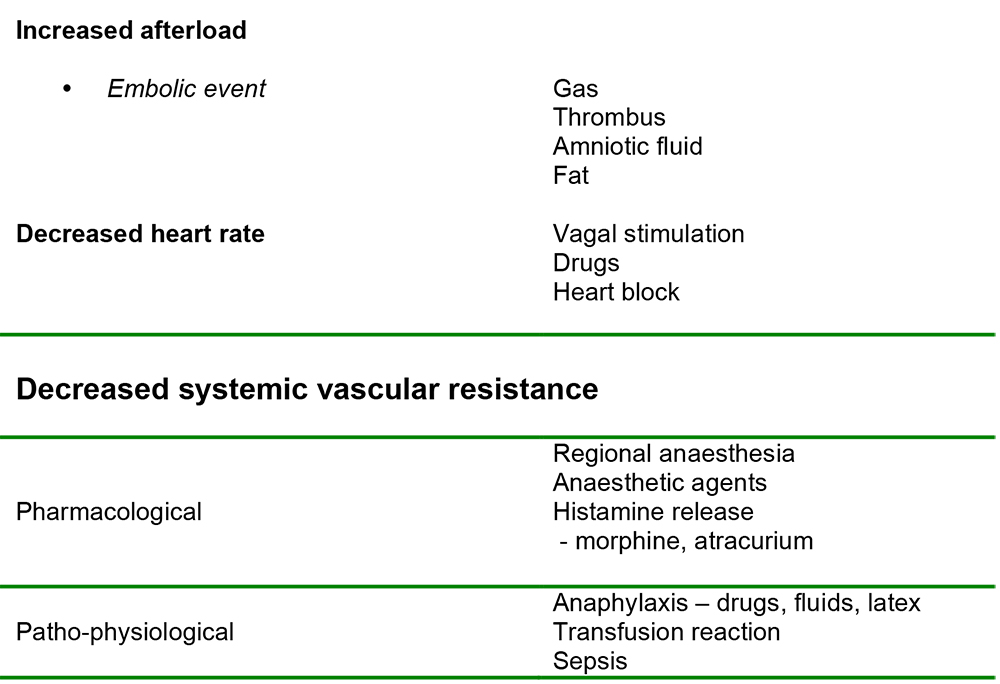
When considering the differentials in clinical practice, it may be useful to categorise them according to patient, surgical and anaesthetic factors. An alternative approach is to consider the underlying physiology as in table 1.
This list is not exhaustive but may help to generate further specific assessment which yields a diagnosis. Conversely, hypotension may result from several contributory causes.
The Australian Incident Monitoring Study (AIMS), which is an ongoing study involving the voluntary reporting of any unintended incident which harms or has potential to harm the patient, reported 438 incidents of significant hypotension from the first 4000 incidents registered in the study. The most common identified causes were drugs in 26% (predominantly intravenous anaesthetic agents, opioids and vaporiser incidents), regional anaesthesia (14%) and hypovolaemia (9%). In 17% of cases the hypotension was attributed to more than one cause. The most common combination identified was hypovolaemia and neuraxial anaesthesia.
PRESENTATION
Morris et al2 noted that hypotension occurred in the absence of heart rate or rhythm changes in 36% cases. In the remainder, hypotension was accompanied by a tachycardia or tachydysrhythmia (9%), bradycardia (31%), or critically with cardiac arrest in 25% cases. Clearly, these co-existing signs may be indicative of the cause, or demonstrate a pattern associated with a particular differential diagnosis.
For example, hypotension as a feature of a pulmonary embolism may be accompanied by tachycardia, raised CVP, cyanosis and bronchospasm. Further clues towards a diagnosis might include chest pain in the awake patient. Evidence of a high regional block may include dyspnoea, upper limb weakness and the development of a Horner’s syndrome. Warm peripheries indicate vasodilatation, suggesting anaesthetic drugs or sepsis as possible causes.
The AIM study observed that accompanying abnormalities in ventilation were seen in 21% cases. Airway complications as the major event, however, were usually associated with a normotensive bradycardia.
MANAGEMENT
The immediate management of a severe hypotensive episode should follow the general guidelines as for any anaesthetic emergency:
- Call for assistance
- Inform the surgical team and discuss possible causes
- Administer 100% oxygen and ensure effective manual ventilation of the lungs (if under general anaesthetic)
- Reduce volatile agent / TIVA (whilst avoiding awareness)
- Make a rapid assessment of ABC and institute specific treatment
This usually involves one or more of the following to improve cardiac output and increase systemic vascular resistance:
- Optimise preload: administer an intravenous fluid bolus e.g. 10 ml / kg crystalloid or colloid, and assess the response. Elevation of legs or head down tilt also improves venous return
- Increase contractility: administer ephedrine
- Systemic vasoconstriction: administer vasoconstrictor e.g. metaraminol, ephedrine
In the event of anaphylaxis, major haemorrhage, cardiac arrest and any other emergency for which a treatment protocol exists, ensure you are familiar with local hospital or national guidelines.
Several measures can also be taken to enhance contractility by ensuring the patient is well oxygenated, normocapnic, normothermic and any acidosis is corrected.
Further management may therefore include:
- Further intravenous fluid boluses and/or blood products
- Vasopressors / inotropic support
- Establishing second large bore intravenous access
- Sending bloods for full blood count / coagulation / cross-match if necessary
- Discussion with haematologist if major haemorrhage suspected
- Drug therapy specific to the cause e.g. anaphylaxis
- Invasive haemodynamic monitoring
This will include frequent re-assessment and review of any corrective interventions.
SYMPATHOMIMETIC DRUGS
Although ephedrine and metaraminol are commonly used as first line treatment, to a certain extent the choice of agent depends on local preferences. Drugs used to increase blood pressure can be broadly divided into those which are predominantly vasopressors and those which are positive inotropes (although there is a significant overlap):
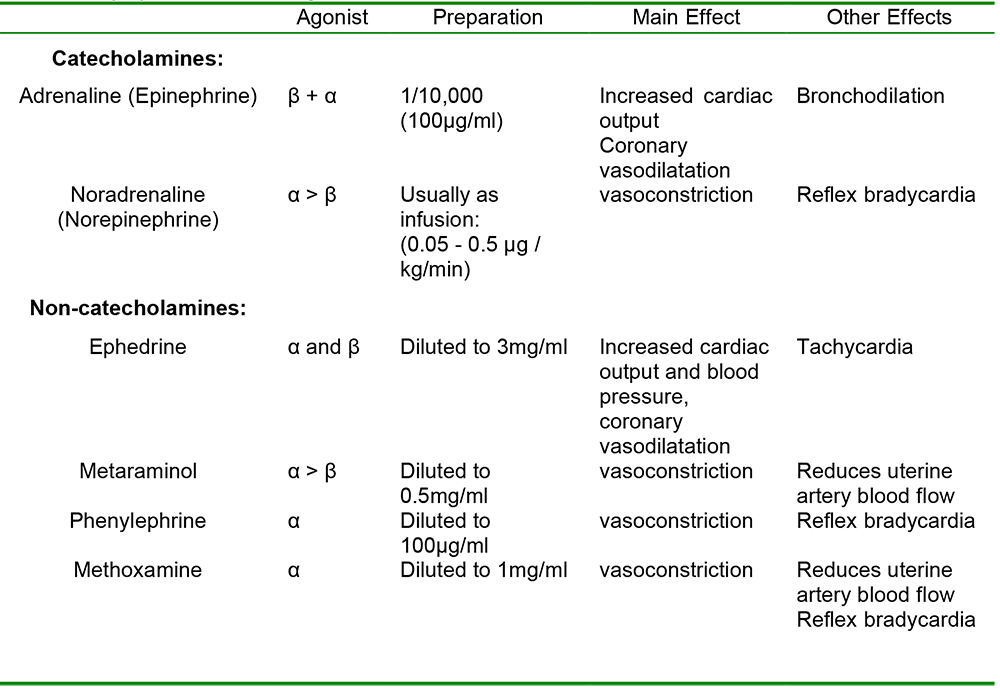
Table 2. Sympathomimetic drugs
SUMMARY
Intraoperative hypotension is usually defined as a mean arterial pressure less than 25% of the patient’s usual value. Untreated, it may result in inadequate organ perfusion. Hypotension may be due to a low cardiac output, low systemic vascular resistance or a combination of both. Risk factors include chronic hypertension and advanced age. The most common causes of intraoperative hypotension are anaesthetic drugs (including regional anaesthesia) and hypovolaemia. Initial management usually involves fluid bolus to optimise preload, and use of drugs to increase contractility and provide vasoconstriction. Thorough evaluation of the patient is required to identify specific underlying causes.
REFERENCES
- Pinnock, C., Lin, T., Smith, T. Fundamentals of Anaesthesia. Second Edition 2003.
- Morris, R.W., Watterson, L.M., Westhorpe, R.N. Crisis management during anaesthesia: hypotension. Quality and Safety in Health Care 2005; 14 e11.
- Yentis, S.M., Hirsch, N.P., Smith, G.B. Anaesthesia and Intensive Care A to Z. Second Edition 2000.
- Allman, K.G., Wilson, I.H. Oxford Handbook of Anaesthesia. 2002
- Aitkenhead, A.R., Rowbotham, D.J., Smith, G. Textbook of Anaesthesia. Fourth edition 2001
- Peck, T.E., William, M. Pharmacology for Anaesthesia and Intensive Care. 2002



