Pain
KEY POINTS
• Low-back pain (LBP) is defined as pain and discomfort from the below the costal margin and above the inferior gluteal folds, with or without leg pain.
• LBP encompasses several types of pain (nociceptive, neuropathic, nociplastic) that may overlap in certain conditions.
• An accurate history and systematic, well-conducted physical examination may give an impression of the cause of the patient’s LBP.
• LBP accompanied by “red flags” warrant imaging and, possibly, more thorough investigation and aggressive management.
INTRODUCTION
Low-back pain (LBP) is pain in the lumbosacral region extending distal from the costal margin to above the inferior gluteal folds, with or without leg pain.1 The term low-back pain is actually a syndrome, a constellation of signs and symptoms,2 which can be caused by known specific pathology such as infection, tumour, ankylosing spondylitis or fracture. However, in some cases, a clear underlying cause is not elucidated. LBP encompasses several types of pain (nociceptive, neuropathic, nociplastic, nonspecific) that may overlap.3 Nociceptive pain results from activation of nociceptors triggered by actual or threatening damage to nonneural tissue or pain caused by activation of peripheral terminals of primary afferent neurons in response to stimuli. Stimuli may be mechanical, noxious chemical or thermal. Neuropathic pain is pain caused by a primary lesion or disease of the somatosensory nervous system.4 Nociplastic pain is a new category of pain, primarily caused by sensitisation of the central nervous system. The pain subtypes usually overlap, with the patient manifesting signs and symptoms of more than one subtype.3
Several clinical practice guidelines recommend triaging patients who present with LBP into 3 categories:
(1) nonspecific LBP, (2) specific mechanical LBP and (3) radicular pain (neuropathic).
LBP cases that are not attributed to recognisable, known specific pathology are classified under nonspecific LBP.1,3 Radicular LBP is pain that extends into the knee, usually below the knee. Lumbar radiculopathy, or radicular LBP in the lumbar area, is a common type of neuropathic pain.4 This is in contrast to axial LBP, which is localised to the low back without radiation to the extremities.
LBP can also be classified by the duration of symptoms. It is classified as acute if an episode persists for less than 6 weeks, subacute if it persists from 6 to 12 weeks and chronic if it persists for 12 weeks or more.1 This classification, however, does not reflect ‘chronification’, the process of conversion of acute to chronic pain.2 Chronification may be determined by eliciting a history of loss of mobility, decreased function, abnormal perception, mood and cognition and pain-related behaviour. Changes in social interaction and occupational difficulties may also be reported by the patient.
LBP is the leading cause of productivity loss and is also the leading cause of years lived with disability worldwide.3,5 The prevalence of LBP increases with age, with a peak of 29% to 41% in patients 40 to 69 years old.
PATHOGENESIS
Potential Causes of LBP
The potential causes of LBP are as follows3:
• Specific mechanical pain
– Disc degeneration
– Facet arthropathy
– Myofascial pain
– Sacroiliac joint arthropathy
– Spondyloarthropathies
– Vertebral body fractures, microfractures, endplate degeneration
• Radicular (neuropathic) pain
– Herniated disc
– Spinal stenosis
– Neoplasm6
> Metastatic carcinoma (most common spinal tumour)
> Benign spinal lesions
~ Osteoid osteoma in lumbar spine
– Osteoblastoma
– Aneurysmal bone cyst
– Spinal giant cell tumour
– Eosinophilic granuloma
> Malignant spinal lesions
– Hematopoietic neoplasm (eg, plasmacytoma, lymphoma)
– Chordoma
– Chondrosarcoma
– Osteosarcoma
– Ewing’s sarcoma and neuroectodermal tumour
– Angiosarcoma
• Infections
– Herpes zoster
– Pyogenic spondylodiskitis/vertebral disc osteomyelitis
• Nociplastic pain7
– LBP with nociplastic component (mixed pain with nociceptive and neuropathic)
– Probable cause of chronic LBP of unknown causes
• Other
– Referred pain from visceral organs (abdominal aortic aneurysm, gastrointestinal, renal, pelvic pain)8
CLINICAL EVALUATION
Recognition of the pain pattern in the clinical evaluation of LBP is important and depends on history, physical examination and response to the anticipated treatment.9
History Taking
A large proportion of LBP cases are nonspecific and resolve without a formal diagnosis, but most guidelines recommend taking the patient’s history to identify specific causes.3 Identifying the pain generators of a patient’s LBP is important for proper planning for treatment. It is essential to determine whether mechanical back pain is present and exclude the “red flags” that could result in permanent damage or a threat to the patient’s life if left untreated.
General Evaluation: Using the PQRST Mnemonic
- Provoking/relieving factors
- Quality (description)
- Region/radiation (Where is the pain? Back pain dominant or leg pain dominant? Does it radiate? Pain anywhere else?)
- Severity (numerical rating scale, visual analogue scale; How much for the back pain? How much for the leg pain?)
- Timing (How long has the patient had the pain? Improving or worsening?)
The patient’s bowel and bladder function should also be assessed, as disturbances in these (ie, incontinence or retention) may indicate the need for urgent intervention. In addition to these symptoms, saddle and/or genital sensory disturbances or sexual dysfunction may be possible presentations of cauda equina syndrome (CES).10 CES generally requires prompt and appropriate surgical management to prevent further worsening and minimise irreversible sequelae.
Risk factors for developing LBP11:
- Genetic factors
- Female sex
- Sedentary lifestyle
- Obesity
- Smoking
- Psychosocial factors (poor social support, anxiety, depression, catastrophising)
- Poor coping mechanisms
- Occupational hazards
- Secondary gain
- Greater disease burden (eg, higher baseline pain, greater disability, and opioid use)
Red Flags and Yellow Flags
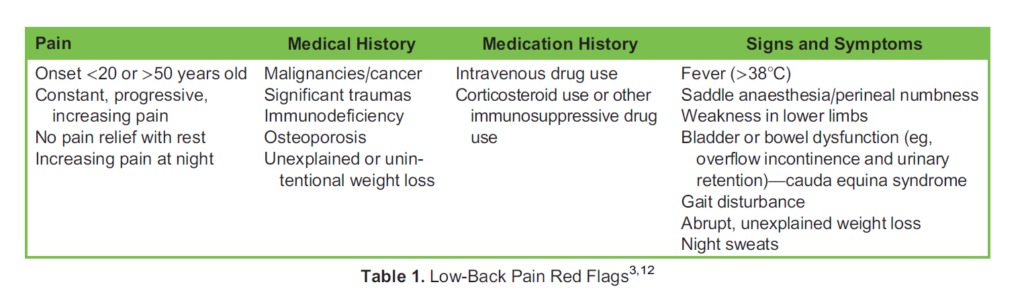
Red flag signs and symptoms identify whether there is risk for the serious diseases.11 History taking and full examination should be taken for diagnostic triage. Several guidelines recommend imaging in patients with ‘red flags’ (Table 1).
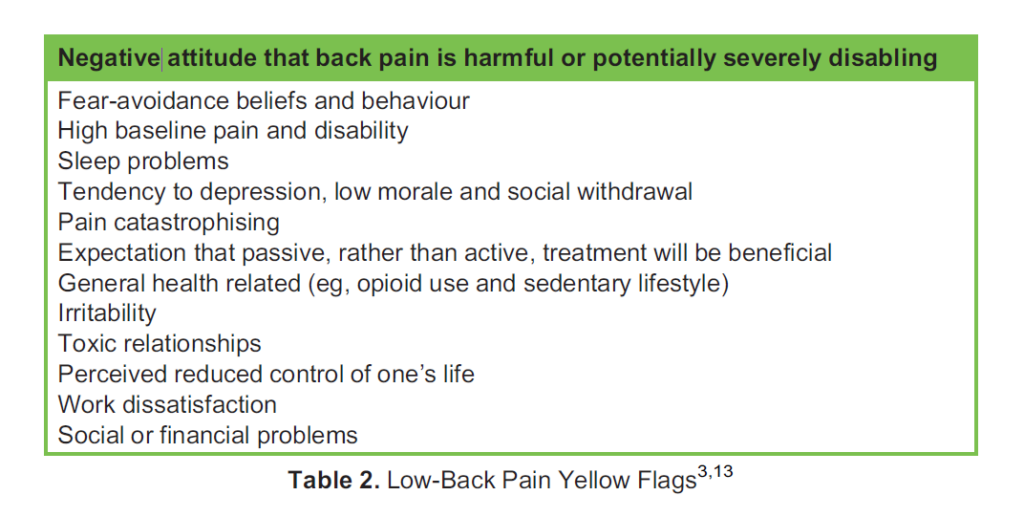
In addition, patients should also be evaluated for psychological and social comorbidities, called ‘yellow flags’ (Table 2), for possible further psychological or social evaluation for the comprehensive management of the condition.
Physical Examination
1. Inspection: Inspect gait when patient is moving around, the patient’s activities, scars from spine surgery, spinal alignment and contour, positioning and avoidance of some postures that aggravate pain.
2. Range of motion: Flexion, extension, rotation and lateral bending aggravated pain; should be correlated to clinical history. Hip joints and other joints should also be evaluated as part of the differential diagnosis.
3. Palpation: The following points of tenderness may suggest the corresponding pathology:
- Spinous process (spondylolisthesis)
- Paraspinal muscles (muscle spasms, trigger point and facet joint pain)
- Greater trochanter (greater trochanter syndrome, osteoarthritis of the hip)
- Posterior superior iliac spine (sacroiliac joint [SIJ] pain)
- Gluteal area (piriformis myofascial pain/tendinopathy)
4. Neurologic examination:
- Motor strength.
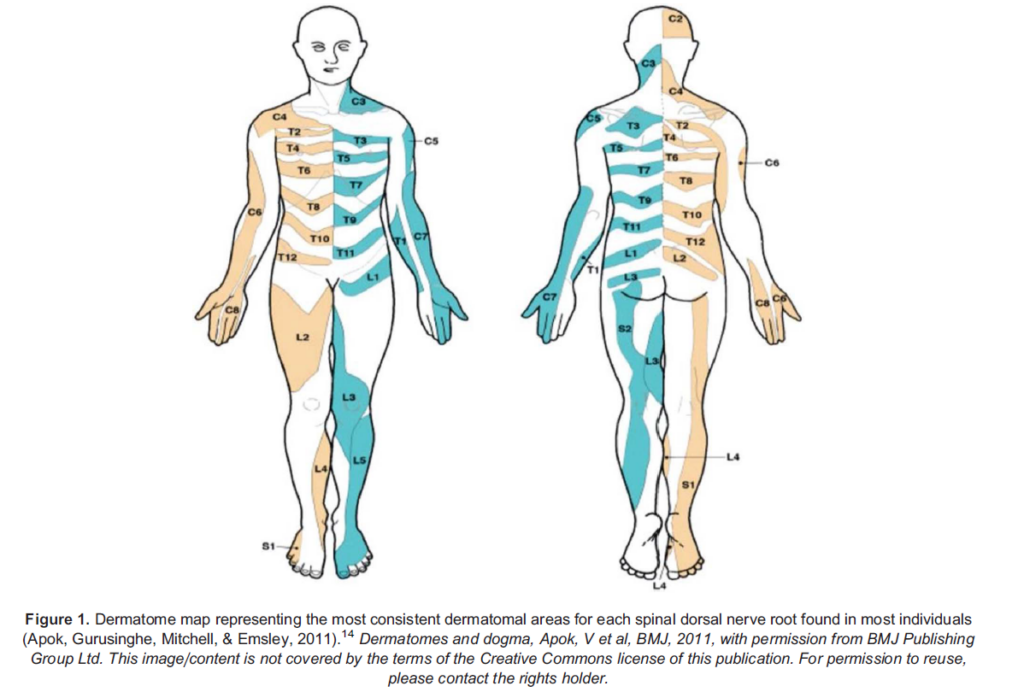
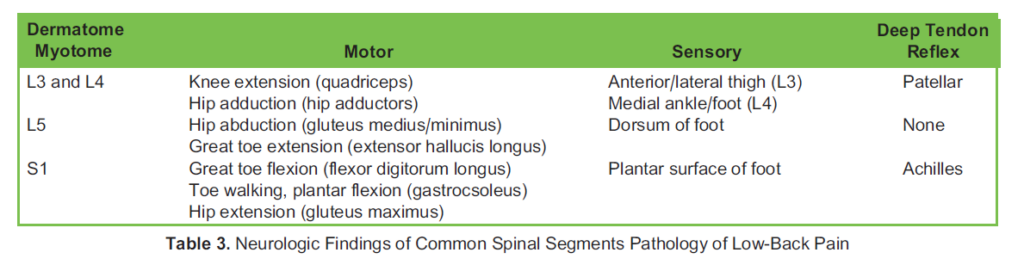
- Sensory: Light touch and pinprick sensation should be assessed in a dermatomal pattern (see Figure 1).14 Determining the pain pattern may identify the specific nerve root causing the patient’s symptoms.
- Reflexes: Diminished reflexes may indicate nerve root compression. Hyperreflexia may suggest an upper motor neuron lesion in the central nervous system. A dermatome map representing dermatomal areas for each spinal dorsal nerve root is shown in Figure 1, while the corresponding nerve responsible for common spinal segment pathology is shown in Table 3.
- A digital rectal examination, which assesses spinal roots S2-4, may be indicated as a part of sacral nerve evaluation in cases such as suspected CES.
5. Provocative tests
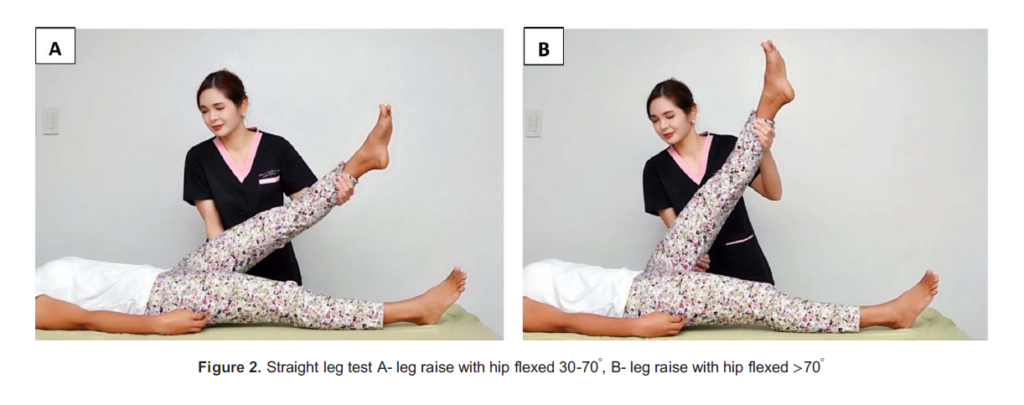
- Straight leg raising (SLR) test/Lasegue test (Figure 2; sensitivity 87%-95%, specificity 22%-35%)15 for nerve root compression/ dural tension of L4-S2. It is considered to be positive when radiating pain along the sciatic nerve, and below the knee, occurs when the hip is flexed at 30 to 708.15
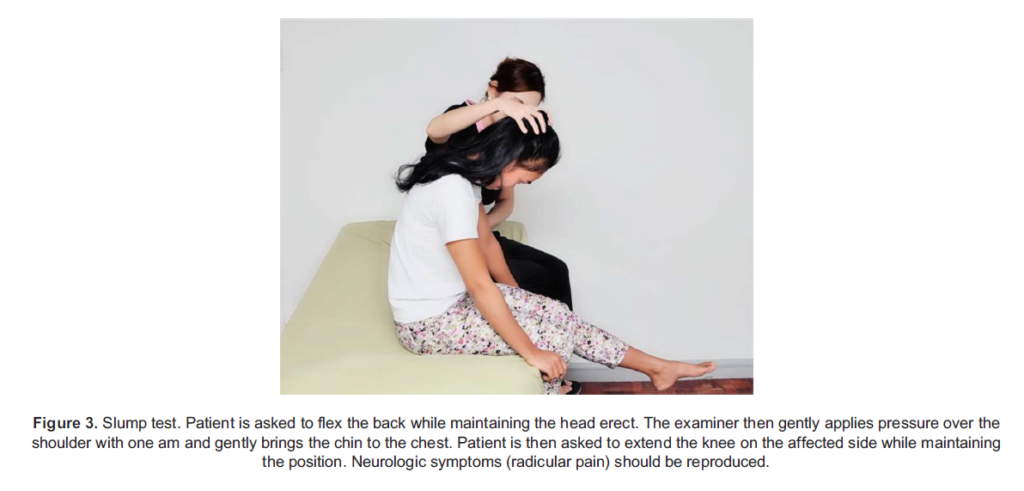
- Slump test (Figure 3): More useful when lower lumbrosacral nerve roots are involved. More sensitive than the SLR test.
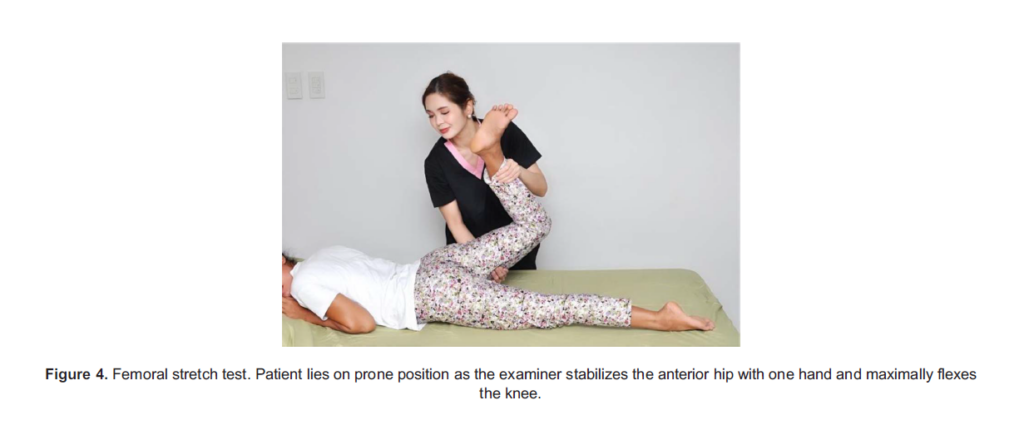
- Femoral stretch test (Figure 4): Mimics upper lumbar nerve (L2, L3, L4) root irritation.
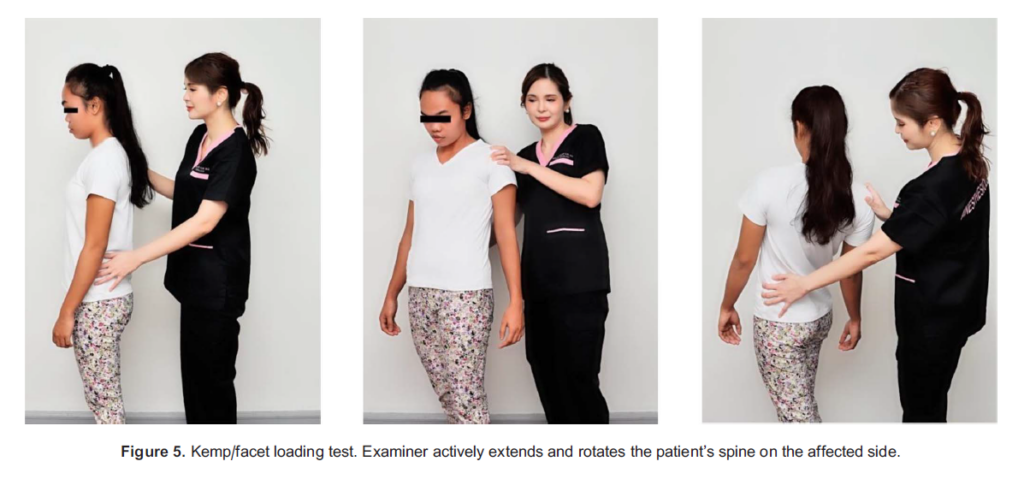
- Kemp/facet loading test (sensitivity 85.7%, specificity 21.8%) (Figure 5)15 for axial back pain. Pain is worse with hyperextension, and the pain can be produced in the patient with passive extension rotation test.
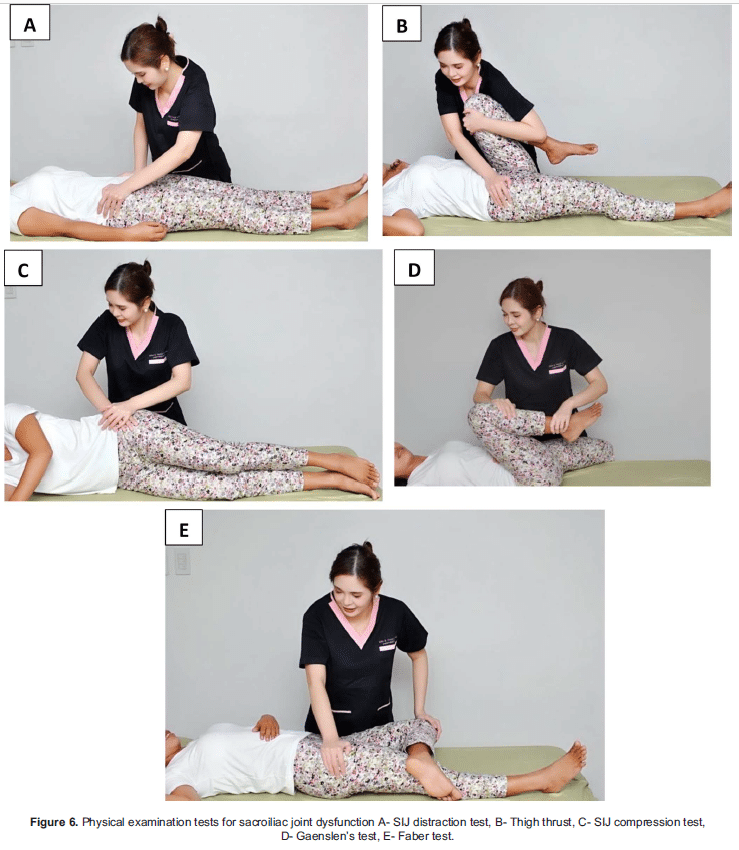
- SIJ provocative tests such as (Figure 6): SIJ distraction test, thigh thrust, Gaenslen test, SIJ compression test, Faber test): 3 or more positive tests provide 91% sensitivity, 78% specificity for sacroiliac joint dysfunction.16 Although some components of the physical examination and provocative tests (ie, facet loading test, SI joint provocative tests) provide moderate specificity for diagnosis, they should be considered as a screening tool. The gold standard for the diagnosis of facet arthropathy17 and SIJ dysfunction18 are the diagnostic blocks (medial branch block and SIJ injection, respectively).
6. Physical examination of other possible pain generators that can cause back pain (ie, hip examination for hip pathology, tender spot survey for fibromyalgia).
DIAGNOSTIC IMAGING
Spine Imaging
In most patients with LBP, imaging modalities are unnecessary and can be delayed for at least 1 month, unless there is a red flag. Anatomical information obtained from imaging studies may not be helpful in identifying the cause of pain and treatment plan. Incidental abnormal findings in imaging modalities can be found in an asymptomatic patient and may lead to unwarranted workup and unnecessary costs. Early imaging is indicated in patients with red flag conditions (Table 1). Imaging modalities support clinical findings by giving visualisation of vertebral alignment, mobility, disc disease, facet disease or fractures of the spine.
1. Plain film X-ray (2 dimensions): used primarily to image bony anatomy
- Initial imaging consists of 2 views, anteroposterior and lateral
- Additional imaging views (lateral oblique, flexion and extension) can be obtained in patients with instability, history of prior fusion and confirmation of finding in initial films.
2. Computed tomography (CT): 2- or 3-dimensional method provides multiplanar viewing capabilities. It is superior for imaging bony anatomy, metastases to the spine and rapid assessment of trauma.
3. Magnetic resonance imaging (MRI): best for evaluation of neural and soft tissue. Tissue differentiation and characterisation are better than CT but poor for bony anatomy. MRI is also advantageous because it does not subject patients to ionizing radiation. Gadolinium (MRI contrast medium) is needed in patients who are suspected to have tumours or infection. It is also helpful for patients who have had previous surgery, as it aids in distinguishing scar tissue from recurrent disc herniation.
TREATMENT
Although most cases of LBP usually resolve with treatment such as rest or taking over-the-counter medications, some end up progressing to chronic LBP.19 These patients need further investigations and extended treatments including interventional techniques.
Acute LBP
Patient Education The goal of treatment of acute LBP is prevention of chronification.2 The treatment of acute LBP, after ruling out specific causes, starts with counselling the patient and providing information to manage the pain. Everyday activities should be continued or resumed, which is termed ‘active recovery’. The patient should be informed that the pain may recur, but behaviour may influence the symptoms and their consequences.
Nonpharmacologic Treatments Exercise therapy is no more effective than the continuation of normal activity in acute LBP.2 Reduced activity and bed rest were found to either have no effect or result in worsening of pain and thus should be avoided. Cognitive behavioural therapy (CBT) may be offered to patients with subacute nonspecific LBP with psychosocial risk factors (‘yellow flags’; see Table 2) for chronification.2
Medication
In patients with acute nonspecific LBP, oral traditional nonsteroidal anti-inflammatory drugs (t-NSAIDs) are recommended to be given in the proper doses with monitoring of side effects.2 COX-2 inhibitors can be given if t-NSAIDs are contraindicated. NSAIDs should be given at the lowest effective dose for the shortest possible duration. Paracetamol alone is not effective for acute LBP.11 A short course of weak opioids, including tramadol, may be given with close clinical follow-up. For LBP caused by specific conditions, medications would depend on the diagnosis.
Chronic LBP
Patient Education Patient education provides long-term reassurance and reduces subsequent primary care visits for low back pain.11 Providers should understand patient expectations and reassure them that recovery is challenging. Maximum pain reduction and return of function are the main goals. Patients should maintain their usual daily life activities and exercise increasingly as tolerated. However, back exercise during the acute phase may worsen symptoms. Heavy exercise should be avoided.
Medication
Medical treatment is similar for various pathologies. Evidence-supported pharmacologic treatments for chronic axial LBP include paracetamol, NSAIDs and selective serotonin-noradrenaline reuptake inhibitors (SNRIs), such as duloxetine. Similar to recommendations for acute LBP, paracetamol should not be offered as monotherapy.11 Anticonvulsants (gabapentin, pregabalin) and antidepressants (tricyclic antidepressants and SNRIs) may be given to patients with radicular pain3.
Nonpharmacologic Treatments
Integrative and multidisciplinary treatment including physical therapy and exercise combined with medication are an ideal approach for chronic LBP. Exercises that follow exercise physiology, traditional mind-body exercises (tai chi, yoga), precise control of movement and bodily awareness (Pilates, motor control exercise, Alexander technique) and exercises that incorporate psychological principles are effective.11 CBT as part of multimodal treatment was also shown to be effective. Massage and acupuncture, however, have mixed support in effectiveness for nonspecific LBP.
Procedural Interventions
Procedural interventions are indicated for patients with LBP that does not resolve within a specific time frame despite medication. The treatment should target the specific pain generators. Interventional techniques have been described with multiple benefits, including pain relief that outlasts the pharmacologic action of local anaesthetics and other agents used. With appropriate patient selection, there is strong evidence to support the benefit of pain interventions in terms of pain control, decreased opioid use and improved function.
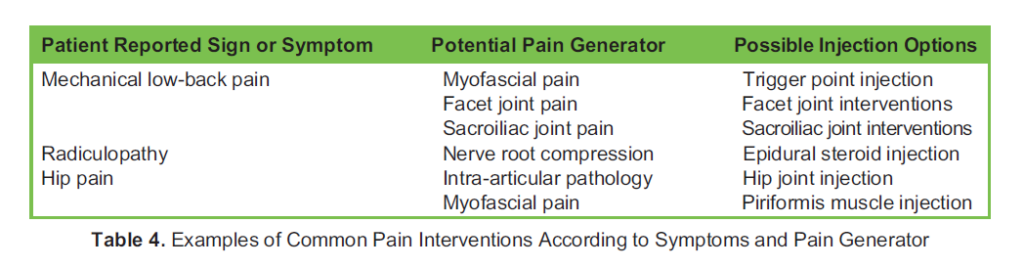
Common pain interventions appropriate for certain symptoms and pain generators are listed are shown in Table 4. The level of evidence supporting some interventions are listed in the Appendix. Surgical intervention may be warranted in some patients. The indications for surgical intervention include constant pain despite appropriate conservative treatment, significant neuro- logic deficit such as cauda equina syndrome, and significant weakness and/or spinal instability.
CONCLUSION
The syndrome of LBP can be classified as nonspecific LBP, specific mechanical LBP and radicular pain. LBP may also be classified based on chronicity of the symptoms. Careful history, physical examination and imaging studies (if warranted) may help in the proper diagnosis and management of patients with LBP. Red flags and yellow flags should be identified in patients with LBP. Most cases are nonspecific and may resolve after resting and taking over-the-counter medications. Acute and chronic LBP cases have different nonpharmacologic and pharmacologic management.
REFERENCES
1. Burton AK, Balague´ F, Cardon G, et al. COST B13 Working Group on Guidelines for Prevention in Low Back Pain. Chapter
2. European guidelines for prevention in low back pain: November 2004. Eur Spine J. 2006;15(suppl 2):S136-S168.
2. Casser HR, Seddigh S, Rauuschmann M. Acute lumbar back pain. Dtsch Arztebl Int. 2016;113(13):223-224.
3. Knezevic NN, Candido KD, Vlaeyen JWS, et al. Low back pain. Lancet. 2021;398(10294):78-92.
4. Nijs J, Apeldoorn A, Hallergraeff H, et al. Low back pain: guidelines for the clinical classification. Pain Phys. 2015;18:E333- E346.
5. Wu A, March L, Zheng X, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8(6):299.
6. Klineberg E, Demicco R, Mazanec D, et al. Masquerade: medical causes of low back pain. Cleveland Clinic J Med. 2007; 74(12):905-913.
7. Nguyen TT, Thelen JC, Bhatt AA. Bone up on spinal osseous lesions: a case review series. Insights Imaging. 2007; 11(80):1-20.
8. Fitzcharles MA, Cohen SP, Clauw DJ, et al. Nociplastic pain: towards an understanding of prevalent pain conditions. Lancet. 2021;397:2098-2110.
9. Hall H. Effective spine triage: patterns of pain. Ochsner J. 2014;14(1):88-95.
10. Gardner A, Gardner E, Morley T. Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J. 2011;20(5):690-697.
11. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736-747.
12. Verhagen AP, Downie A, Popal N, et al. Red flags presented in current low back pain guidelines: a review. Eur Spine J. 2016;25(9):2788-2802.
13. Samanta J, Kendall J, Samanta A. Chronic low back pain. BMJ. 2003;326:535.
14. Apok V, Gurusinghe NT, Mitchell JD, et al. Dermatomes and dogma. Pract Neurol. 2011;11:100-105.
15. Kwong EH, Virani N, Robert M, et al. Inter-rater reliability of the active straight-leg raise and one-leg standing tests in nonpregnant women. J Rehab Med. 2013;45(10):1058-1064.
16. Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16(3):142-152.
17. Datta S, Lee M, Falco FJ, et al. Systematic assessment of diagnostic accuracy and therapeutic utility of lumbar facet joint interventions. Pain Physician. 2009;12(2):437-460.
18. Chuang C, Hung S, Pan P, et al. Diagnosis and interventional pain management options for sacroiliac joint pain. Tzu Chi Med J. 2019;31(4):207-210.
19. Casiano VE, Sarwan G, Dydyk AM, et al. Back pain. Updated 2023 February 20. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. https://www.ncbi.nlm.nih.gov/books/NBK538173/
20. Laslett M, McDonald B, Aprill C, et al. Clinical predictors of screening lumbar zygapophyseal joint blocks: development of clinical prediction rules. Spine J. 2006;6:370-379.
21. Huygen F, Kallewaard JW, van Tulder M, et al. Evidence-based interventional pain medicine according to clinical diagnoses: update 2018. Pain Pract. 2019;19:664-675.
22. Sayed D, Grider J, Strand N, et al. The American Society of Pain and Neuroscience (ASPN) evidence-based clinical guideline of interventional treatments for low back pain. J Pain Res. 2022;15:3729-3832.
23. Manchikanti L, Kaye AD, Falco FJE, et al, eds. Essentials of Interventional Techniques in Managing Chronic Pain. 1st ed. Cham, Switzerland: Springer International Publishing; 2018.
APPENDIX
1. Facet joint interventions
a. Facet joint injection (level I/strong)17
b. Medial branch block (level II/moderate)17
c. Radiofrequency ablation (weak evidence)20
2. Epidural steroid injections
a. Transforaminal (level I-A for treatment of low-back and radicular pain originating from disc disease, spinal stenosis and for chronic back/leg pain after surgical intervention)21,22
b. Interlaminar (level I-A for low-back and radicular pain originating from disc disease, spinal stenosis and for chronic back/ leg pain after surgical intervention)21,22
c. Caudal epidural steroid injection (level I-A for treatment of low back and radicular pain originating from disc disease, spinal stenosis and for chronic back/leg pain after surgical intervention when interlaminar or transforaminal approaches are not feasible)22
3. Trigger point injections (TPI) for low-back pain (LBP) secondary to myofascial pain syndrome (MPS)
a. The type of medication does not make a significant difference in pain outcomes (level I-A)22
b. Eliciting a localised twitch response for needle placement predicts best outcomes (level I-A)22
c. In medically refractory cases, TPI with botulinum toxin-A may be of benefit (level I-B)22
d. Dilute local anaesthetic concentrations may result in less injection pain (level II)22
e. Novel injectables may be of benefit for MPS (level II)22
f. Adjunct therapies (ie, physiotherapy) may be of use to prolong the relief of TPI for MPS (level II)22
4. Sacroiliac joint interventions
a. Sacroiliac joint injection—intra-articular and periarticular steroid injection (limited to poor evidence)16
b. Sacral lateral branch radiofrequency ablation (very weak evidence)23
5. Intradiscal regenerative therapies for discogenic LBP
a. Intradiscal platelet-rich plasma injection (level I-B)22
b. Intradiscal allogenic mesenchymal stem cells (MSC) (level I-B)22
c. Intradiscal bone marrow–derived MSC (level I-B)22
d. Intradiscal adipose tissue–derived MSC (level I-C)22



