Obstetrics Anaesthesia
INTRODUCTION
Key Points
- Physiology commonly deteriorates progressively in critically ill obstetric patients
- Identification of abnormal physiological parameters and early intervention may prevent further deterioration and reduce maternal morbidity and mortality
- Obstetric Warning Scores may help identify pregnant women at risk of deterioration
- The Maternal Early Warning Score (MEWS) is a commonly used example of a bedside screening tool that enables tracking of physiological parameters, and when a predefined threshold is reached, triggers bedside assessment by a healthcare professional
According to Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries in the UK (MBRRACE-UK) report 2016, maternal mortality rate is 8.5 per 100,000 maternities.1 More than 50% of maternal deaths are potentially preventable.2 Nine pregnant women develop severe maternal morbidity for every maternal death.3 Evolving morbidity can be difficult to recognise in the obstetric population because of the normal changes in peripartum physiology. Delays in recognition of patient deterioration and initiation of treatment lead to worse outcomes.2
Early Warning Systems (EWS) have been used since 1999 in the general patient population to identify clinical deterioration.4 The Maternal Early Warning System (MEWS) has been advocated with the aim to reduce maternal morbidity and mortality, and improve clinical outcomes.1 The MEWS tracks physiological parameters and evolving morbidity and once a predetermined threshold has been reached, it triggers evaluation by a healthcare professional. The healthcare professional determines further evaluation, treatment or intervention as necessary.
Many variations of obstetric EWSs are currently in use: such as the Modified Obstetric Early Warning System (MOEWS), the Maternal Early Warning Trigger tool (MEWT) and the Irish Maternal Early Warning System (IMEWS). For the purpose of this article, all early warning scores and systems in the obstetric population are referred to as Maternal Early Warning Score (MEWS), unless otherwise specified.
The Centre for Maternal and Child Enquiries (CEMACE) report in 2011 recommended the introduction of MEWS to all maternity units in the United Kingdom.2 MEWS tools have also been recommended by the Association of Anaesthetists of Great Britain and Ireland, the Obstetric Anaesthetists’ Association in the UK, the Health Information and Quality Authority in Ireland and the National Partnership for Maternal Safety in the United States.
THE NON-OBSTETRIC EXPERIENCE
EWSs have been in used in clinical practice since 1999 in non-obstetric patient populations.4 This commonly involves a triggering system based on physiological parameters, where one or more values trigger a response. Sometimes an aggregate scoring system is used where physiological parameters are assigned a value and the total score determines the response. A response consists of the regular recording of vital signs made by the nurse, recognising when thresholds have been reached, alerting a healthcare professional and requesting bedside evaluation. EWSs have been studied in paediatric, medical and surgical populations. In adult medical and surgical cohorts, a systematic review showed an abnormal EWS reliably predicted death (AUROC*,0.88-0.93) and cardiac arrests (AUROC*, 0.74-0.86).5 The impact of EWSs on preventing adverse outcomes was not clear.5
A National Early Warning Score (NEWS) was introduced in the UK in 2012.6 The national system standardised care and clinical management, simplified communication, and is important for research validation.
When considering effectiveness of EWSs, sensitivity and specificity are important. A system with high false positives may place increased demands on clinical services, cause alarm fatigue and lead to unnecessary interventions. In addition to being valid and reliable, an effective EWS should be tailored to the specific clinical setting.6
*Area Under the Receiver Operating Characteristic curve
THE OBSTETRIC EXPERIENCE
Maternal Early Warning Scores
Due to normal physiological changes of pregnancy, the EWS for the non-obstetric population is not directly transferrable to the obstetric population.7 The MEWS was designed to account for the normal physiological changes of pregnancy. The intention of the MEWS is to improve recognition of pregnant women at risk of clinical deterioration and facilitate early intervention.1 Triggers in the MEWS system theoretically lead to earlier recognition of conditions that can contribute to maternal morbidity and mortality, including cardiovascular disease, sepsis, thromboembolic disease, haemorrhage and pre-eclampsia.1 The MEWS is intended to guide clinical judgement, and not replace it.
MEWS are now extensively used in obstetric practice, but the systems in use vary significantly.8 The parameters commonly included in MEWS are heart rate, respiratory rate, blood pressure and level of consciousness (table 1). Other parameters such as the pain score, lochia characteristics and urine output are sometimes included, either in the score or recorded on the chart. Table 1 is an example of various physiological parameters recorded as normal, yellow or red, depending on how abnormal the value is compared to normal pregnancy physiology. Figure 1 gives an example of an escalation protocol of appropriate interventions for triggering pregnant women. Of note, if the care provider is concerned about the pregnant women, she should be discussed with senior medical staff irrespective of MEWS.
In addition to identifying patients at risk, MEWS also improve the reliability of taking and recording a full set of vital signs, e.g. respiratory rate is often not measured or recorded. Respiratory rate is one of the more sensitive parameters when trying to identify patients at risk of deterioration.11 A MEWS facilitates communication and provides an expectation and auditable standard for response by the medical team to deterioration in a pregnant woman’s physiology.
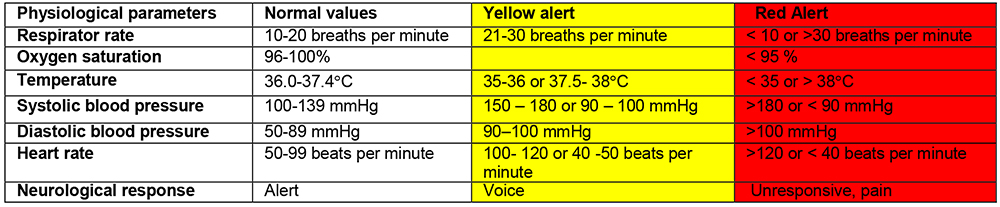
Table 1: Maternal Early Warning Scores
EVIDENCE FOR MEWS
The literature suggests potential benefit and supports the use of MEWS. A prospective observational study published in 2016 evaluating a MEWS reported that 27% of women triggered a response, and 17% of women fulfilled criteria for obstetric morbidity.9 The MEWS was found to be 86% sensitive and 85% specific for predicting the presence of maternal morbidity.9
A study that compared the predictive value of six different MEWSs at identifying severe sepsis in women with chorioamnionitis reported a sensitivity range of 40%-100% and a specificity range of 4%-97%.10 The authors concluded that MEWS tools with simpler designs tended to be more sensitive, whereas the more complex ones were more specific, and suggest that further research is needed.10 Simple scores are more reliable, are less prone to human calculation errors and have increased reproducibility.11
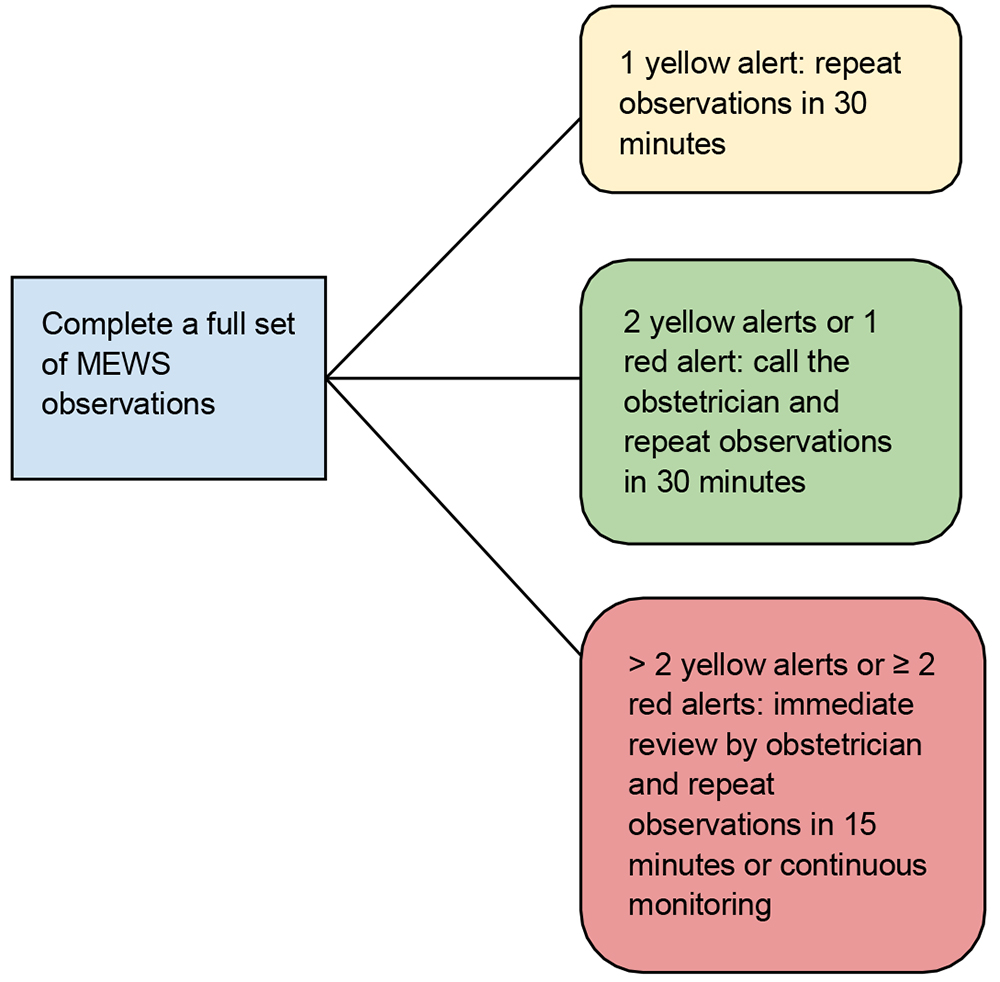
Figure 1: Obstetric Early Warning Score Escalation Protocol
In 2013, the Intensive Care National Audit and Research Center (ICNARC) in the UK reported the first statistically validated early warning scoring system for pregnant women.11 A dataset of obstetric admissions to the intensive care unit (ICU) were analysed and the ICNARC MEWS was compared to pre-existing MEWSs, in their ability to predict survival based on physiological parameters in the first 24 hours in the ICU.11 The ICNARC MEWS was found to have a high sensitivity and specificity, with AUROC curve of 0.94 (95% CI 0.88 – 0.99).11
A prospective study carried out over multiple sites within a large hospital system provides evidence for an alternative MEWS tool, the Maternal Early Warning Trigger (MEWT).12 Introduction and use of the tool in over 180,000 deliveries showed a 14% (p = 0.01) reduction in composite maternal morbidity and an 18% (p = 0.01) reduction in severe maternal morbidity (as defined by the Centres for Disease Control and Prevention).12
CONCLUSION
MEWSs are a promising tool for reducing maternal morbidity and mortality. In order to improve health outcomes, MEWSs should identify patients at risk of deterioration at a time when early intervention can prevent progression to severe morbidity. Currently there is no evidence or consensus on optimum parameters or trigger levels for obstetric patients.
Further research is needed to determine the optimum MEWS.10 Establishment of a nationally standardised MEWS would potentially provide the necessary data to analyse and refine parameters in order to improve sensitivity and specificity. However, different institutions may benefit by tailoring trigger parameters and actions depending on the resources available. The MEWS is only a part of the management of a critically ill pregnant woman. Outcomes will depend on appropriate escalation of care and management provided when MEWS trigger.
SUMMARY
Maternal morbidity and mortality reports have found that clinical response to acute physiological deterioration in pregnant women is at times delayed, and this is associated with poor outcomes.2 The MEWS is a screening tool intended to improve the response to a physiological deterioration in the pregnant patient and facilitate early intervention. Future research should focus on validation, parameter refinement, resource allocation, and cost effectiveness of MEWS.
REFERENCES
- Knight M, Nair M, Tuffnell D, et al. on behalf of MBRRACE-UK. Saving Lives, Improving Mothers’ Care – Surveillance of maternal deaths in the UK 2012-14 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009-14. Oxford: National Perinatal Epidemiology Unit, University of Oxford 2016. https://www.npeu.ox.ac.uk/downloads/files/mbrrace-uk/reports/MBRRACEUK%20Maternal% 20Report%202016%20-%20website.pdf [last accessed 20/05/18]
- Centre for Maternal and Child Enquiries (CMACE). Saving Mothers’ Lives: reviewing maternal deaths to make motherhood safer: 2006–08. The Eighth Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. Br J Obstet Gynaecol 2011;118 (Suppl. 1):1–203
- Nelligan PJ, Laffey JG. Clinical review: Critical care in pregnancy. Crit Care 2011;15:1014
- Goldhill DR, White SA, Sumner A. Physiological values and procedures in the 24 h before ICU admission from the ward. Anaesthesia 1999;54:529 – 534
- Smith ME, Chiovaro JC, O’Neil M, et al. Early Warning System Scores for Clinical Deterioration in Hospitalised Patients: A Systematic Review. Ann Am Thoracic Soc 2014;11:1454–65
- Royal College of Physicians. National Early Warning Score (NEWS): Standardising the assessment of acute illness severity in the NHS. Report of a working party. London: RCP, 2012
- Institute of Obstetricians and Gynaecologists, Royal College of Physicians of Ireland and Directorate of Clinical Strategy and Programmes, Health Service Executive. Clinical Practice Guideline: The Irish Maternity Early Warning System (IMEWS) https://www.hse.ie/eng/services/publications/clinical-strategy-andprogrammes/ imews-guidelines.pdf
- Isaacs R, Wee MYK, Bick D, et al. A national survey of obstetric early warning systems in the United Kingdom: five years on. Anaesthesia 2014;69:678- 692
- Singh A, Guleria K, Vaid NB, et al. Evaluation of maternal early obstetric warning system (MEOWS chart) as a predictor of obstetric morbidity: a prospective observational study. Eur J Ob Gynecol Reproduct Biol. 2016;207:11-17
- Edwards SE, Grobman WA, Lappen JR et al. Modified obstetric early warning scoring systems (MOEWS): validating the diagnostic performance for severe sepsis in women with chorioamnionitis. Am J Obstet Gynecol. 2015 Apr;212(4):536.e1-8
- Carle C, Alexander P, Columb M, et al. Design and internal validation of an obstetric early warning score: Secondary analysis of the Intensive Care National Audit and Research Centre Case Mix Programme database. Anaesthesia. 2013;68(4):354–367
- Shields LE, Wiesner S, Klein C et al. Use of Maternal Early Warning Trigger tool reduces maternal morbidity. Am J Obs Gynaecol. 2016;214:527.e1-6



