Regional Anaesthesia
KEY POINTS
- Knowledge of the nerve supply to the knee joint is essential to choose the appropriate nerve blocks to anaesthetise the whole knee.
- The articular nerves that supply the knee are mainly branches from the femoral (FN), obturator (ON) and sciatic nerve (SN).
- Adductor canal or femoral triangle blocks are used to anaesthetise nerves covering the anterior aspect of the knee without clinical significant motor block.
- The IPACK block is used to anaesthetise articular branches of the posterior part of the knee while sparing motor branches.
- Local infiltration analgesia is another motor-sparing technique but is performed by the surgeon in 3 different stages during the surgery, aiming to cover the anterior and posterior parts of the knee.
INTRODUCTION
In this article, we describe motor-sparing techniques to block the nerves supplying the knee, in line with enhanced recovery pathways that encourage early postoperative mobilisation.
Total knee arthroplasty (TKA) is one of the most commonly performed and painful orthopaedic procedures. According to the National Joint Registry, more than 100000 TKAs are carried out in the United Kingdom every year, with a mean patient age of 68.9 years.1 Effective analgesia and early ambulation in these patients is essential to reduce complications and improve outcomes.
Multimodal analgesia incorporating regional anaesthesia techniques provides optimum analgesia and minimises the use of opioids and their side effects. Proximal nerve blocks such as the lumbar plexus, femoral nerve and proximal sciatic nerve blocks provide excellent analgesia but frequently cause motor weakness, which reduces the patient’s mobility and leads to a risk of falls.2 Motor-sparing techniques should theoretically provide the optimum balance between analgesia and mobility. A thorough understanding of the innervation of the knee joint will enable us to provide effective regional anaesthesia following knee surgeries without motor weakness.
INNERVATION OF THE KNEE
The innervation of the knee joint is complex and follows Hilton’s law. This law states that the nerve supplying the muscles that lie across a joint not only supplies those muscles but also supplies the joint beneath and the skin overlying those muscles. The articular nerves that supply the knee are derived from the femoral (FN), obturator (ON) and sciatic nerve (SN) via the tibial (TN) and common peroneal nerve (CPN).
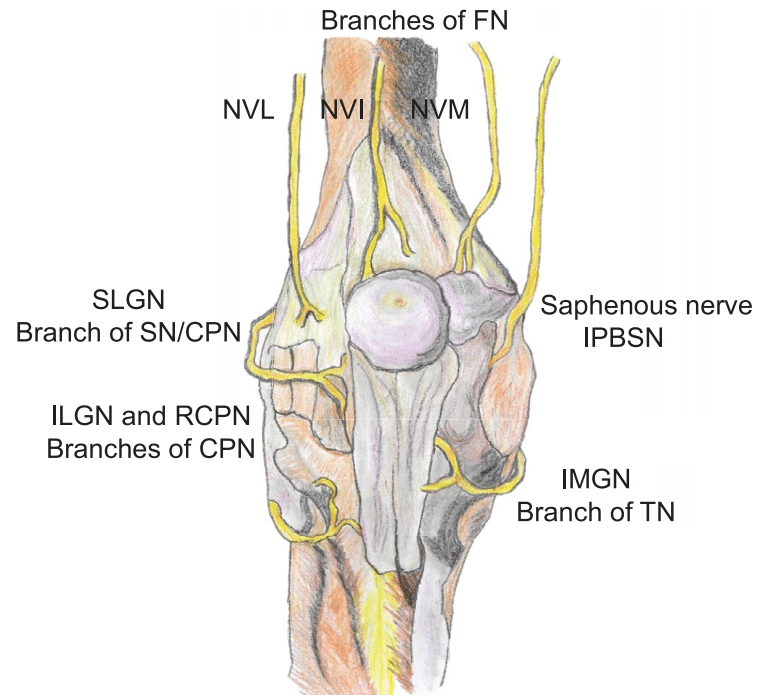
Figure 1. Main nerves providing articular branches for the innervation of the anterior capsule of the knee. FN, femoral nerve; TN, tibial nerve;
CPN, common peroneal nerve; SN, sciatic nerve; NVL, nerve to vastus lateralis; NVI, nerve to vastus intermedius; NVM, nerve to vastus
medialis; SLGN, superior lateral genicular nerve; ILGN, inferior lateral genicular nerve; RCPN, recurrent branch of the common peroneal nerve;
IPBSN, infrapatellar branch of the saphenous nerve; IMGN, inferior medial genicular nerve.
Sensory Supply of the Anterior Knee Capsule
The sensory nerve supply to the anterior knee is mainly derived from branches of the FN, CPN and TN, with minor and inconsistent contributions from the ON and lateral femoral cutaneous nerves. The sensory supply to the knee is best understood by dividing it into 4 quadrants (see Figures 1 and 2).
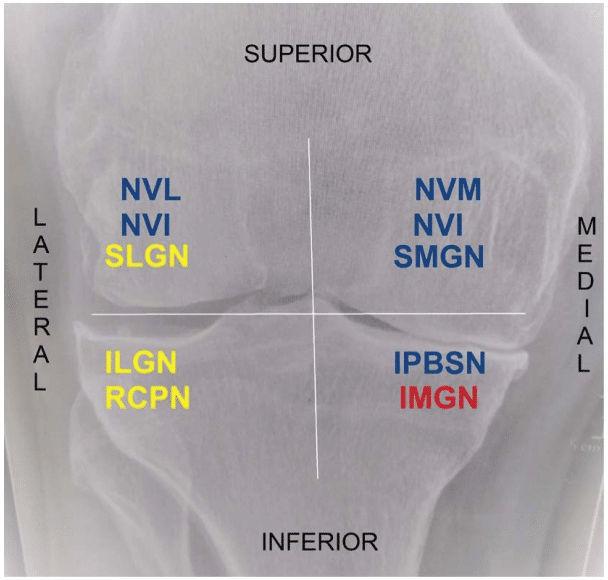
Figure 2. Main nerve branches innervating the anterior knee joint divided into 4 quadrants. Blue: branches of the femoral nerve; yellow:
branches of the common peroneal nerve/sciatic nerve; red: branch of the tibial nerve. NVL, nerve to vastus lateralis; NVI, nerve to vastus
intermedius; NVM, nerve to vastus medialis; SLGN, superior lateral genicular nerve; SMGN, superior medial genicular nerve; ILGN, inferior
lateral genicular nerve; RCPN, recurrent branch of the common peroneal nerve; IPBSN, infrapatellar branch of the saphenous nerve; IMGN,
inferior medial genicular nerve.
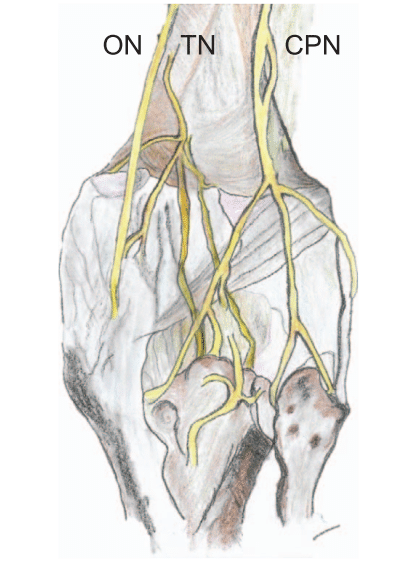
Figure 3. Main nerves providing articular branches for the innervation of the posterior capsule of the knee. TN, tibial nerve; ON, obturator
nerve; CPN, common peroneal nerve.
The superolateral anterior aspect of the knee capsule is supplied by the nerves to the vastus lateralis and vastus intermedius (both are branches of the FN), by the superior lateral genicular nerve (either a branch of the CPN or SN) and by the CPN itself.3
The superomedial anterior aspect of the knee capsule is innervated by the nerve to vastus medialis (NVM), the vastus intermedius nerve and the superior medial genicular nerve, all of which are branches of the FN.3
The inferolateral anterior aspect of the knee capsule is supplied by 2 branches of the CPN: the recurrent branch of the CPN and the inferior lateral genicular nerve.
The superior part of the inferomedial anterior aspect of the capsule is innervated by the infrapatellar branch of the saphenous nerve, which is a branch of the saphenous nerve (SPN; the terminal sensory branch of the FN). The inferior medial genicular nerve, a branch of the TN, supplies the inferior aspect of the inferomedial quadrant of the knee capsule.3
The anterior and posterior branches of the ON sometimes give an additional supply to the cutaneous inferomedial part of the thigh and the anteromedial knee capsule, respectively.4
Sensory Supply of the Posterior Knee Capsule
Posterior knee capsule innervation is mainly mediated by articular branches from the TN and the posterior branch of the ON, with minor contributions from the CPN and the SN5 (see Figure 3).
Branches of the TN supply the entire posterior capsule. These branches course transversely to the intercondylar region between the medial and lateral femoral condyles.
The superomedial aspect of the posterior capsule is also supplied by articular branches from the posterior branch of the ON, which enter the popliteal fossa through the adductor hiatus with the femoral artery (FA) and vein.
The superolateral aspect of the posterior capsule can be additionally supplied by articular branches from the SN and CPN.
All of these articular branches travel through a tissue space between the popliteal artery (PA) and the femur to innervate the posterior capsule of the knee. The aim of the Infiltration between Popliteal Artery and Capsule of the Knee (IPACK) block is to infiltrate local anaesthetic (LA) in this plane to anaesthetise these articular branches.
MOTOR-SPARING BLOCKS FOR THE KNEE
Anterior Knee: Femoral Triangle and Adductor Canal Blocks
A femoral nerve block is well established as providing excellent analgesia to the anterior knee following TKA by covering almost the entire anterior capsule, muscles and cutaneous innervation of the anterior thigh and knee.4 However, the use of large doses of LA or continuous infusions have been shown to cause quadriceps weakness and reduce mobility postoperatively.6
The adductor canal (AC) block was proposed as an alternative to the femoral nerve block to decrease the risk of quadriceps weakness whilst still providing good analgesia after knee operations. It was described using ultrasound at the midpoint between the anterior superior iliac spine and the base of the patella on the medial aspect of the thigh to identify and block the SPN adjacent to the FA and spare blockade of femoral motor branches. However, further research has demonstrated that a block performed as described above would not be in the AC but is likely to be in the distal part of the femoral triangle (FT).7
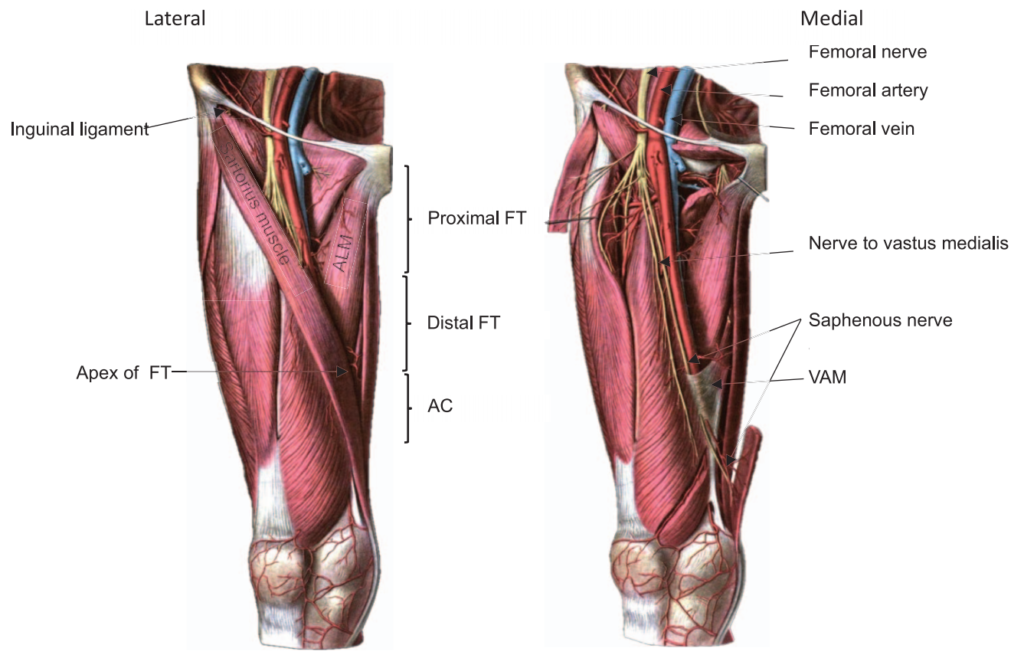
Figure 4. Anatomy of the FT and AC.9 FN, femoral nerve; FA, femoral artery; FV, femoral vein; FT, femoral triangle; AC, adductor canal; ALM,
adductor longus muscle; VAM, vasoadductor membrane. Original ultrasound images from the authors.
This differentiation is important, as the deposit of LA in these 2 places would also lead to a different analgesic effect. A block performed in the true AC would mainly block the SPN (which is the only nerve that consistently runs inside the AC) and in some cases the posterior branch of the ON.4 However, the block performed in the distal part of the FT (see the FT block below) would block the SPN, the NVM (which contributes significantly to the innervation of the anteromedial knee joint) and nerves supplying the cutaneous dermatomes of the knee such as the medial femoral cutaneous nerve4 but providing similar motor sparing to AC blocks.8
It is therefore crucial to clarify some basic anatomical concepts and be aware of the use of inconsistent and/or imprecise terminology.
The FT is formed by the inguinal ligament at its base and the intersection of the medial borders of the sartorius and adductor longus muscles at its apex.7 The FT can be further divided into a proximal and distal portion, at the intersection of the medial border of the sartorius muscle and the lateral border of the adductor longus muscle. This point corresponds with the point where the sartorius muscle begins to cover the femoral neurovascular bundle.4 The end of the FT at its apex marks the beginning of the AC, which ends at the adductor hiatus, where the FA and femoral vein become the PA and popliteal vein4,7 (see Figure 4).
How to Do FT and AC Blocks
Before starting any block, obtain consent from the patient, ensure the correct side is marked, prepare equipment, have a skilled assistant and resuscitation drugs available, apply patient monitoring, gain intravenous access and carry out a ‘‘stop before you block.’’
The patient is positioned supine with the knee slightly flexed and the hip externally rotated (‘frog leg’ position). A pillow can be placed behind the patient’s knee for comfort. The transducer is placed anteromedially, approximately at the middle of the thigh, to identify the FA below the sartorius muscle. The probe is then moved proximally and distally, keeping the FA in the middle of the screen until the apex of the FT is identified at the point where the medial borders of the sartorius and the adductor longus muscles meet7 (see Figure 5).
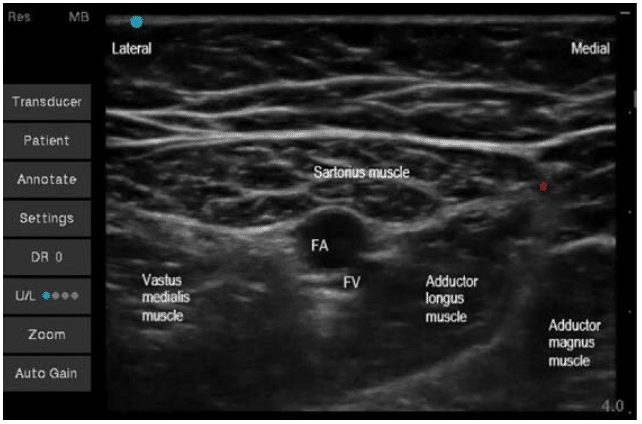
Figure 5. Ultrasound image showing the apex of the FT. *Shows the point at which the medial borders of the sartorius and adductor longus
muscles meet. FT, femoral triangle; FA, femoral artery; FV, femoral vein.
FT Block
Once the apex of the FT is identified, the probe is moved slightly proximal, and the LA is injected anterolateral to the FA below the sartorius muscle (subsartorial). At this point, the SPN and NVM can usually be identified as hyperechoic structures lateral to the FA (see Figure 6). It is important to ensure that the injection is made cephalic to the apex of the FT but where the FA is covered by the sartorius muscle (meaning the distal FT; see Figure 4) to avoid blocking motor branches given off in the proximal FT.4 To reduce the risk of proximal spread, the use of large volumes (>20 mL) of LA is not recommended.
AC Block
To perform a true AC block, the LA should be injected distally to the apex of the FT but proximally to the end of the AC, which is identified by the femoral vessels exiting the adductor hiatus to become the popliteal vessels (see ATOTW 301, ‘‘UltrasoundGuided Adductor Canal Glock (Saphenous Nerve Block)’’). 10
For both the FT and AC blocks, low concentrations of a long-acting LA (for example, levobupivacaine 0,25%) are used to avoid motor block but provide prolonged analgesia. For analgesia of knee surgery, we recommend an FT block and low volumes of LA (<20 mL)
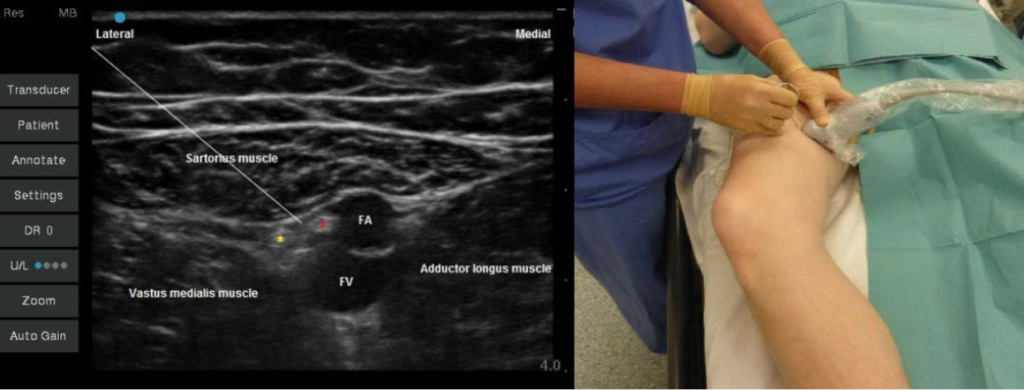
Figure 6. Ultrasound image of the distal FT block and positioning the patient in the ‘frog leg’ position. The yellow * indicates the nerve to vastus
medialis. The red * indicates the saphenous nerve. FT, femoral triangle; FA, femoral artery; FV, femoral vein. —demonstrates the needle
trajectory.
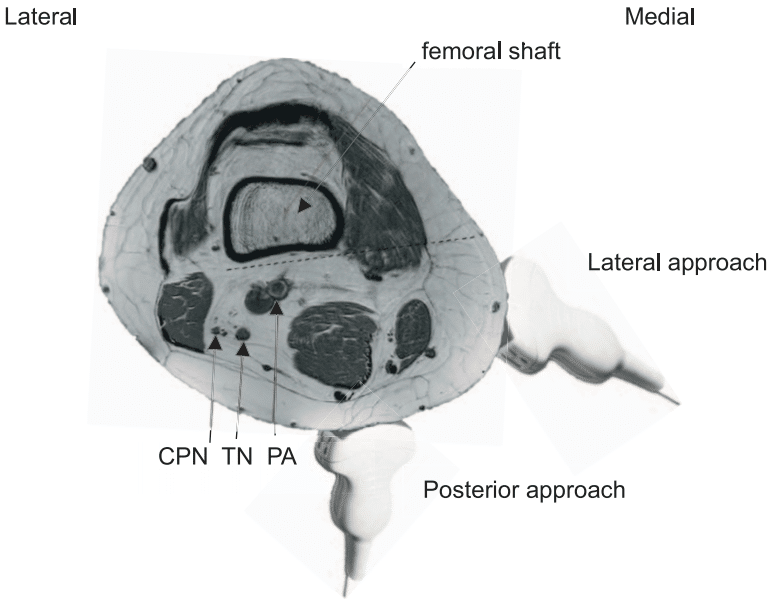
Figure 7. Magnetic resonance image of the interspace between the popliteal artery and the femoral shaft where the local anaesthetic is
infiltrated when performing an infiltration between popliteal artery and capsule of the knee block and the probe position when performing lateral
and posterior approaches. — demonstrates the needle trajectory. CPN, common peroneal nerve; TN, tibial nerve; PA, popliteal artery.
Posterior Knee: IPACK Block and Popliteal Plexus Block
IPACK Block
The IPACK block is a novel technique developed by Sinha.11 The IPACK block consists of an infiltration of LA between the PA and the posterior capsule of the knee. The goal of the IPACK block is to anaesthetise the articular branches innervating the posterior knee joint while avoiding the blockade of the TN and CPN and any motor or sensory impairment of the leg and foot.
The optimal LA volume and site of infiltration to reach the greatest number of articular branches is still under discussion12; however, the clinical evidence is based on Sinha’s approach in while the LA is infiltrated at the level immediately superior to the femoral condyles; we referred to this approach here.
How to Do IPACK Blocks
Usually, a curvilinear probe is required to obtain enough depth to view the femur and the PA; a linear probe can be used depending on the patient’s body habitus. Consider the use of full aseptic precautions, as the injection site is very close to the surgical field.
There have been 2 different approaches described to perform IPACK blocks: lateral and posterior. In both approaches, the LA is deposited in the interspace between the PA and the knee capsule using a 100-mm needle from medial to lateral. However, the probe position is different; hence, the view of the needle and interspace are different (see Figure 7).
IPACK: Lateral Approach
The block is performed with the patient in the same position as when performing AC or FT blocks: supine with the knee flexed and the hip externally rotated (‘frog leg’ position). The curvilinear probe is placed on the medial side of the lower third of the thigh to identify the femur and the FA and femoral vein (see Figure 7).
The femoral vessels are then traced distally to observe them diving into the popliteal fossa to become the PA and popliteal vein. Once the PA is identified posterior to the femur, the probe is moved slightly further distally and posterior to get a better view of the interspace between the PA and the shaft of the femur just above the femoral condyles. The needle is inserted from medial to lateral and advanced parallel to the acoustic shadow of the femur between the shaft of the femur and the PA until the tip is placed 2 cm beyond the PA. The LA is injected as the needle is withdrawn after negative aspiration, filling the gap between the PA and the femur (see Figure 8).

Figure 8. Lateral infiltration between popliteal artery and capsule of the knee block. Position of the ultrasound probe and correlating ultrasound
image. PA, popliteal artery. — demonstrates the needle trajectory.
IPACK: Posterior Approach
The block can be performed with the patient in the frog leg, lateral or prone positions. It is logistically easier not to ask the patient to change positions and keep him or her in the frog leg position, as when performing FT or AC blocks.
Regardless of the position of the patient, the probe is placed transversely at the level of the popliteal crease to identify the femoral condyles and the PA (see Figure 7). The femoral condyles are seen as discontinuous curved hyperechoic lines (see Figure 9). Once the femoral condyles and PA are identified, the probe is moved slightly proximal until this discontinuous hyperechoic line changes to a continuous hyperechoic line of the femoral shaft. At this point, just above the femur condyles, the needle is inserted using an in-plane technique, from medial to lateral and parallel to the femoral shaft. The needle is advanced between the femur and PA until the tip is placed 2 cm beyond the PA or near the lateral border of the periosteum. The LA is injected as the needle is withdrawn after negative aspiration and the space is filled. It is good practice to identify, whenever possible, the TN and CPN in the image to be sure to avoid them (see Figure 10).
It is recommended to use a low concentration of a long-acting LA to minimise the risk of motor block but prolong the sensory blockade (for example, levobupivacaine 0,25%). A variable range of 10 to 20 mL of LA is used to infiltrate this tissue plane.
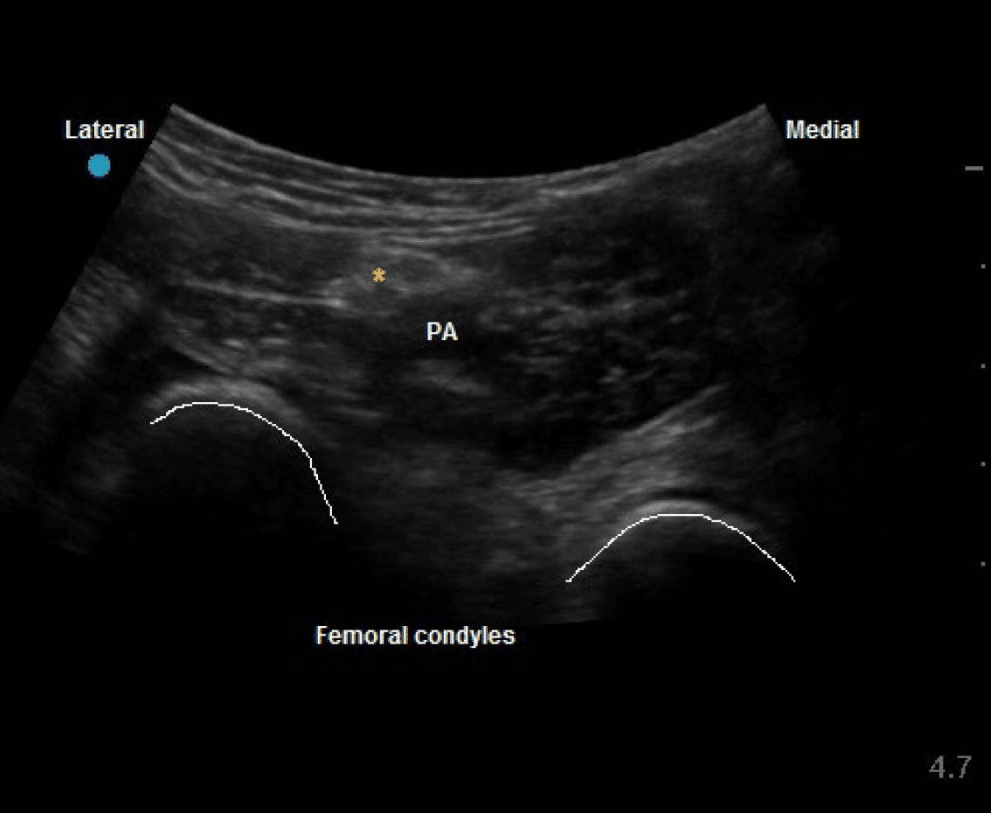
Figure 9. Posterior infiltration between popliteal artery and capsule of the knee approach. Ultrasound image showing the femoral condyles. PA,
popliteal artery. Yellow * indicates the tibial nerve
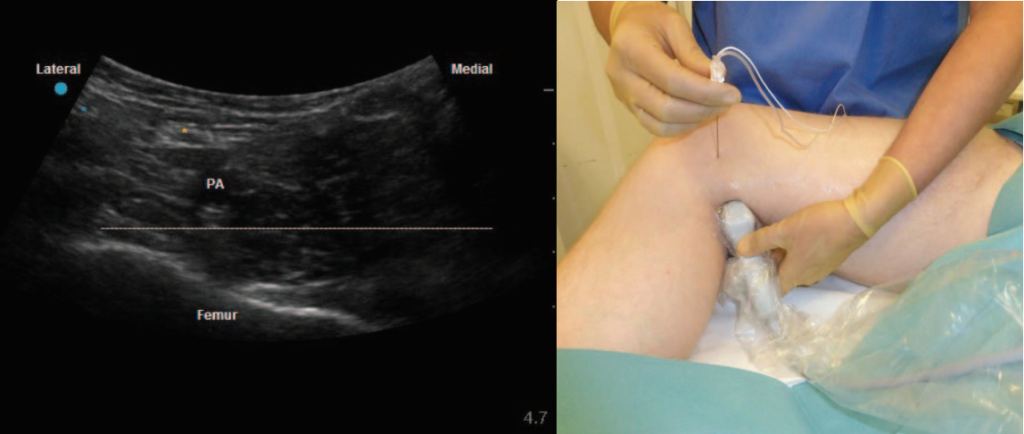
Figure 10. Posterior infiltration between popliteal artery and capsule of the knee approach. Position of the ultrasound probe and corresponding
ultrasound image. Yellow * indicates the tibial nerve. Blue * indicates the common peroneal nerve. PA, popliteal artery. — demonstrates the
needle trajectory.
Popliteal Plexus Block
It has been suggested that the articular branches that innervate the posterior capsule of the knee could also be anaesthetised by the injection of LA at the distal part of AC just before the femoral vessels dive to become popliteal vessels. This approach has been termed the popliteal plexus block.
In cadavers, the injection of dye at this level has spread in the popliteal fossa, staining the popliteal plexus and the posterior obturator nerve. Based on these findings, Runge et al13 showed in a small study that a popliteal plexus block in combination with an FT block provided effective pain relief after TKA. However, further studies are needed to prove its efficacy.
Local or Periarticular Infiltration of Analgesia by Surgeons
Local infiltration analgesia (LIA) involves injection of a mixture of high-volume diluted LA with adjuvants within multiple layers surrounding the knee joint to cover the whole knee. This technique has demonstrated postoperative pain and morphine consumption reduction after TKR.
LIA is usually done in 3 stages. Stage 1 involves injection of 30 to 50 mL of the LIA mixture into the posterior joint capsule from the front. This is injected once the bone has been prepared but before the prosthesis has been inserted, because access to the posterior capsule is limited after this point. Stage 2 involves injection of 35 to 50 mL of LIA mixture into the deep tissues around the medial and lateral collateral ligaments and the wound edges after the prosthesis has been inserted but before the wound is closed. Stage 3 involves injection of 25 to 50 mL of LIA mixture into the subcutaneous tissue, approximately every 25 mm around the wound.14
There are no currently published studies comparing postoperative outcomes after TKR when LIA alone or the combination of FT/AC blocks and IPACK blocks are used.
Ultrasound-Guided Genicular Nerve Blocks
A distal blockade of genicular branches has been also described using ultrasound in acute and chronic pain management. The superior medial genicular nerve and superior lateral genicular nerve can be identified using ultrasound and blocked at the level of the medial and lateral femoral epicondyles deep to the vastus medialis and lateralis, respectively. The inferior medial genicular nerve can be also targeted medial to the tibial plateau adjacent to the genicular vessels.15,16 The blockade of these nerves anaesthetise the superior and inferomedial aspects of the knee, but their feasibility for acute postoperative pain management needs further research.
Continuous Peripheral Nerve Block
A continuous peripheral nerve block can be achieved by inserting a catheter and administering an infusion and/or intermittent boluses of LA. Continuous AC blocks and continuous FT blocks have demonstrated similar pain relief and functional mobilization after TKA.8 However, a continuous AC block provides early ambulation as compared with continuous FN block.6 No studies have been published on continuous IPACK blocks. For further details, refer to ATOTW 412, ‘‘Introduction to Perineural Catheters.’’ 17
CONTRAINDICATIONS AND COMPLICATIONS
Contraindications and complications are the same as for any regional anaesthetic technique. Specific considerations include the following:
- Risk of myotoxicity when continuous AC infusions are used. Although this is rare, there have been a small number of quadriceps weakness cases published, and it should be considered if a delay in mobilization occurs.
- Risk of SPN damage when performing IPACK blocks. There are no case reports yet, but the needle trajectory from the medial side of the distal thigh crosses the anatomical course of the SPN, and this could be inadvertently injured if not avoided.18Risk of foot drop if the LA spreads to the CPN when performing IPACK blocks.10 When possible, the TN and CPN should be identified and intentionally avoided, and the needle should not be advanced more than 2 cm beyond the PA or near the lateral border of the periosteum.
EQUIPMENT
- Ultrasound machine with high-frequency linear and curvilinear probes
- 22-gauge 50- to 100-mm short bevelled insulated ultrasound needle
- Skin antiseptic
- Gloves
- Probe cover
- LA for the block; a safe dose should be calculated based on the patient’s weight, and the concentration may be reduced to allow a sufficient volume when combining multiple blocks
- If a continuous peripheral nerve block is performed, strict aseptic precautions must be used and further equipment is needed:
- Peripheral nerve catheter set
- Pump device for delivery of LA, either electronic or disposable elastomeric pumps
SUMMARY
Regional anaesthesia techniques that promote early ambulation and effective pain relief are essential after TKA. Knowledge of sensory innervation is key to providing the appropriate block for the appropriate surgery. FT blocks provide sensory cover to the anterior knee and sparing clinical significant motor weakness, whilst IPACK blocks anaesthetise the articular branches covering the posterior part of the knee without motor block.
ACKNOWLEDGEMENT
We would like to thank Jose Luis Humanes, Ben Butcher and Charles Bishop for their kind contribution to this tutorial.
REFERENCES
- National Joint Registry Reports. 16th annual report. Accessed November 28, 2019. https://reports.njrcentre.org.uk/
- Johnson R, Kopp S, Hebl J, et al. Falls and major orthopaedic surgery with peripheral nerve blockade: a systematic review and meta-analysis. Br J Anaesth. 2013;110(4):518-528.
- Tran J, Peng PWH, Lam K, et al. Anatomical study of the innervation of anterior knee joint capsule: implication for imageguided intervention. Reg Anesth Pain Med. 2018;43(4):407-414.
- Bendtsen TF, Moriggl B, Chan V, et al. The optimal analgesic block for total knee arthroplasty. J.Reg Anesth Pain Med. 2016;41(6):711-719.
- Tran J, Peng PWH, Gofeld M, et al. Anatomical study of the innervation of posterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med 2019;44:234-238.
- Brick KL Kuang MJ, Ma JX, et al. Is adductor canal block better than femoral nerve block in primary total knee arthroplasty? A GRADE analysis of the evidence through a systematic review and meta-analysis. J Arthroplasty. 2017;32(10):3238-3248.e3.
- Wong W, Bjørn S, Strid J, Børglum J, Bendtsen T. Defining the location of the adductor canal using ultrasound. Reg Anesth Pain Med. 2017;42:241e5.
- Chuan A, Lansdown A, Bourgeois AJG, et al. Adductor canal versus femoral triangle anatomical locations for continuous catheter analgesia after total knee arthroplasty: a multicentre randomised controlled study. Br J Anaesth. 2019;123(3):360-367.
- Sobotta J. Atlas and Text-book of Human Anatomy, Volume III. London, England: W. B. Saunders Company; 1914.
- Quemby D, McEwen A. ATOTW 301. Ultrasound guided adductor canal block (saphenous nerve block). Accessed April 1, 2021. https://resources.wfsahq.org/atotw/ultrasound-guided-adductor-canal-block-saphenous-nerve-block/
- Sinha S. ASRA News. How I do it: infiltration between popliteal artery and capsule of knee (iPACK). Accessed November 28, 2019. https://www.asra.com/asra-news/article/158/how-i-do-it-infiltration-between-poplite
- Tran J, Giron Arango L, Peng P, et al. Evaluation of the iPACK block injectate spread: a cadaveric study. Reg Anesth Pain Med. 2019;rapm-2018-100355.
- Runge C, Bjørn S, Jensen J, et al. The analgesic effect of a popliteal plexus blockade after total knee arthroplasty: a feasibility study [published online May 24, 2018]. Acta Anaesthesiol Scand. doi:10.1111/aas.13145
- Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop. 2008;79(2):174-183.
- Vanneste B, Tomlinson J, Desmet M, et al. Feasibility of an ultrasound-guided approach to radiofrequency ablation of the superolateral, superomedial and inferomedial genicular nerves: a cadaveric study. Reg Anesth Pain Med. 2019;rapm-2019-100381.
- Egeler C, Jayakumar A, Ford S. Motor-sparing knee block—description of a new technique. Anaesthesia. 2013;68(5):542-543.
- Gupta A, Wolmarans M, Ghosh SM. ATOTW 412, ntroduction to Perineural Catheters. Accessed April 14, 202. https://resources.wfsahq.org/atotw/introduction-to-perineural-catheters/
- Sebastian MP, Bykar H, Sell A. Saphenous nerve and IPACK block. Reg Anesth Pain Med. 2019;rapm-2019-100750.



