General Topics
MCQ’s
- During anaesthesia, a patient with Parkinson’s disease on levodopa should not receive:
- enflurane
- fentanyl
- morphine
- droperidol
- nitrous oxide
- Extrapyramidal effects can be seen following the administration of:
- chlorpropamide
- terfenadine
- metoclopramide
- domperidone
- perphenazine
- Recognised causes of abnormal movements of the hands include:
- respiratory failure
- renal failure
- chronic alcoholism
- liver failure
- depigmentation of substantia nigra
- Oral drugs which can be used in the treatment of Parkinson’s disease as first line agents are:
- entacapone
- Levodopa
- Selegiline
- Apomorphine
- pethidine
- Recognised features of Parkinson’s disease are:
- rigidity
- dry mouth
- orthostatic hypotension
- dysphagia
- restrictive ventilatory defect
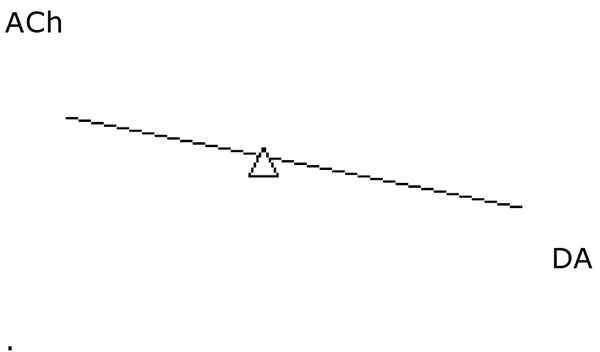
Parkinson’s disease (PD) is a neurological disease involving the extrapyramidal system, with a prevalence of 1% in patients over the age of 65 years. It is characterised by tremor, rigidity and postural instability. Idiopathic Parkinson’s disease is due to loss of dopaminergic neurones in the substantia nigra, causing an imbalance of acetylcholine (Ach) and dopamine (DA). 80% of neurones are lost before the syndrome is clinically apparent.
Aetiology
The aetiology of Parkinson’s disease is idiopathic, but the aetiology of Parkinsonism (clinical conditions which resemble idiopathic Parkinson’s disease) can be:-
- Idiopathic
- Drugs – drugs which block dopamine receptors (eg phenothiazines, butyrophenones, metoclopramide) can cause Parkinsonism. Drugs affecting dopamine synthesis, storage or release (eg reserpine) can also produce the same effect.
- Infarction- post encephalitis, AIDS
- Vascular- arteriosclerosis, multi- infarct disease
- Tumour
- Post trauma eg repeated head injury
- Toxicity eg Wilson’s disease, heavy metals, carbon monoxide poisoning
- Metabolic eg hypoparathyroidism, Wilson’s disease.
Clinical features
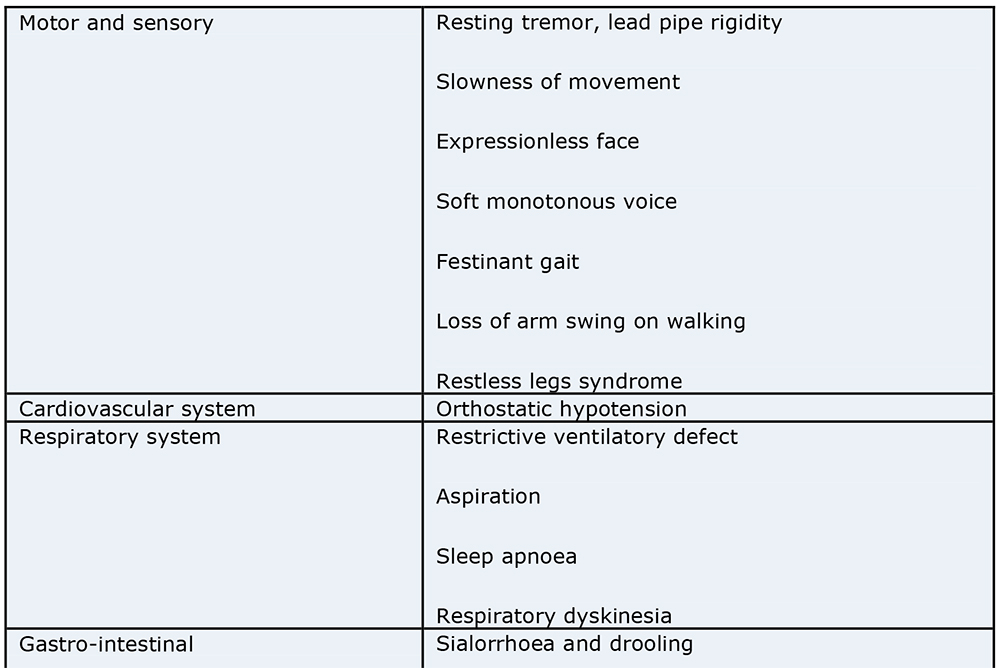
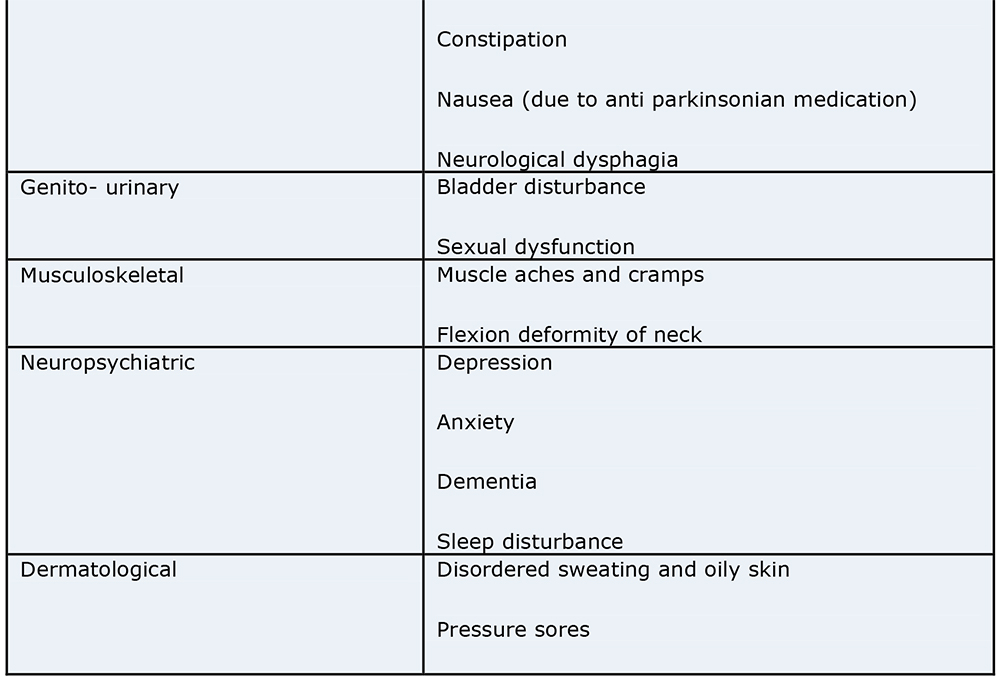
PD is a multi- system disorder :-
Management
There are many drugs available, but the choice of treatment depends on the stage of the disease, side effects of treatment, and patient compliance.
Dopamine precursors (eg levodopa) are converted to dopamine in CNS. Given with a peripherally acting dopa decarboxylase inhibitor (DDI) to reduce systemic breakdown.Anaesthetic cautions– orthostatic hypotension, dyskinesia, NMS (neuroleptic malignancy syndrome). If the patient is not on a DDI , the high dopamine levels can predispose to arrhythmias under general anaesthesia.
Dopamine agonists (eg ropinirole, apomorphine) act by mimicking the action of dopamine at the dopamine receptor.
Mono-amine oxidase Type B inhibitors (MAO-I) eg selegiline – act by preventing breakdown of dopamine in the central nervous system by the enzyme mono-amine oxidase.Anaesthetic cautions- these drugs interact with pethidine causing hypertension and hyperpyrexia.
Anti-cholinergics (eg orphenadrine) – act by antagonising the excitatory effects of cholinergic pathways. Anaesthetic cautions– risk of central anticholinergic syndrome.
Atypical drugs (eg amantadine)
Catechol –O- methyl transferase (COMT) inhibitors – these drugs are used with levodopa and DDI combination to smooth out end of dose “off” periods. Anaesthetic cautions– caution withdrugs which are metabolised by COMT (eg adrenaline).
Drugs and anaesthesia
PD drugs are stopped as late as possible pre-operatively, and are restarted as soon as possible postoperatively. This is difficult if the patient is unable to swallow, or in those who have had major abdominal surgery. Levodopa can be given NG or NJ and is rapidly absorbed in the proximal small bowel. Prolonged GI dysfunction post- operatively may lead to severe disability as there is currently no parenteral dopaminergic therapy available. A subcutaneous apomorphine infusion can be used in those patients in whom there will be a delay in starting anti –PD medication post operatively. Apomorphine acts as a dopamine agonist. Apomorphine is commenced 1-2 days prior to elective surgery. The dose is usually 30-40 mg over 16 hours, but will depend on the response to apomorphine challenge carried out pre- operatively. Domperdione can be given prior to the apomorphine challenge (20 mg tds for 3 days, PR). Apomorphine can cause significant hypotension which may be hazardous in the perioperative period.
Surgical approaches in the treatment of PD have developed due to failure of medical treatment to provide long term relief of the symptoms of PD. Surgery is reserved for those with refractory PD with disabling problems, and does not cure PD. A multidisciplinary approach is used in patient selection for these procedures. DBS (deep brain stimulators) can be used in the the treatment of PD. DBS can be used in the ventral intermediate nucleus, STN (subthalamic nucleus) or GPi (internal segment of globus pallidus). Thalamic stimulation is effective in the relief of tremor, but worsening dysarthria can occur. Subthalamic DBS improves PD symptoms and reduces daily drug intake. GPi stimulation reduces medication side effects, thus leading to better drug tolerance however produces little improvement of bradykinesia or tremor. Alternative surgical options include pallidotomy, subthalamotomy and transplantation.
Anaesthetic considerations
Pre-operative:
- Management should be optimised before surgery
- Anaesthetist should be given advanced warning of patient.
- Liase with the patients Parkinson’s disease physician.
- Put the patient first on the theatre list (as the timing of drug administration is predictable, and also to reduce the chances of the patient being cancelled. If the patient is cancelled then medication should be recommenced).
- Assess the patient- in addition to the usual pre-operative assessment, pay attention to:
- Airway – difficult intubation may occur due to flexion deformity of the neck. These patients are also at high risk of aspiration.
- Sialorrhoea- there may be a need for a drying agent pre- operatively
- Rule out chest infection.
- Pulmonary function testing may reveal a restrictive ventilatory defect.
- Ask about sleep apnoea.
- Autonomic dysfunction.
- Consider the need for HDU/ITU post operatively particularly for those with poor cough, risk of aspiration, sleep apnoea, respiratory inadequacy or autonomic instability. Adequate hydration perioperatively will reduce the risk of orthostatic hypotension.
- Adequate hydration perioperatively will reduce the risk of orthostatic hypotension.
Which drugs are safe for PD patients?
- Opiates are often necessary after major surgery, but may worsen muscle rigidity (it is likely that the amount of morphine used for analgesia is far less than this). Pethidine should be avoided as can cause hypertension and muscle rigidity in patients on selegiline. Patient controlled analgesia (PCA) may be difficult to operate.
- Antidepressants – the use of TCA’s may potentiate levodopa induced arrhythmas.
- Antipsychotics (eg phenothiazines, butyrophenones, piperazine derivatives) may worsen PD symptoms. It is best to use atypical antipsychotics (eg sulpiride, clozapine).
- Antihypertensives may cause severe hypotension in those with PD (due to postural hypotension, hypovolaemia).
- Volatile agents the use of halothane can potentiate levodopa induced arrhythmias.
- Induction agents – propofol may have dopamine like effects, and thus help reduce tremor and muscle rigidity.
- Anticholinergic drugs- centrally acting ones (eg atropine) can precipitate central anticholinergic syndrome. Glycopyrrolate is the anticholinergic of choice.
- Anti-emetics are of importance as nausea/vomiting can hinder restarting enteral PD drugs. The anti emetics that are not safe to use in those with PD are metoclopramide, droperidol and prochlorperazine as these drugs will worsen PD symptoms and cause extra pyramidal effects.
- The anti emetic of choice is domperidone (10- 20 mg 4-6 hourly PO, or 30-60 mg 4-6 hourly PR). Domperidone does not cross the BBB (blood brain barrier) and thus does not cause extra pyramidal effects.
- 5 HT anatagonists (eg ondansetron, granisetron) can be used in those with PD. The use of antihistamine anti-emetics (eg cyclizine) is also safe in those with PD.
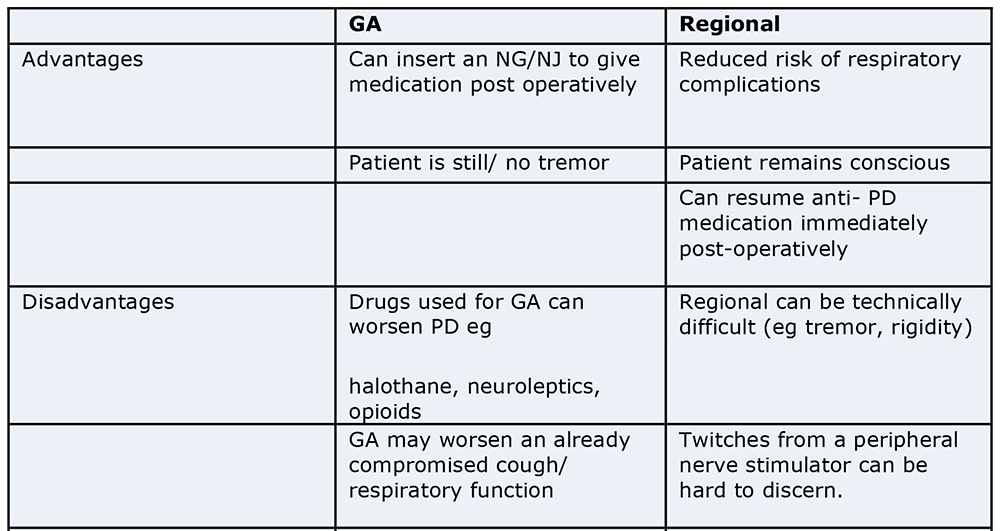
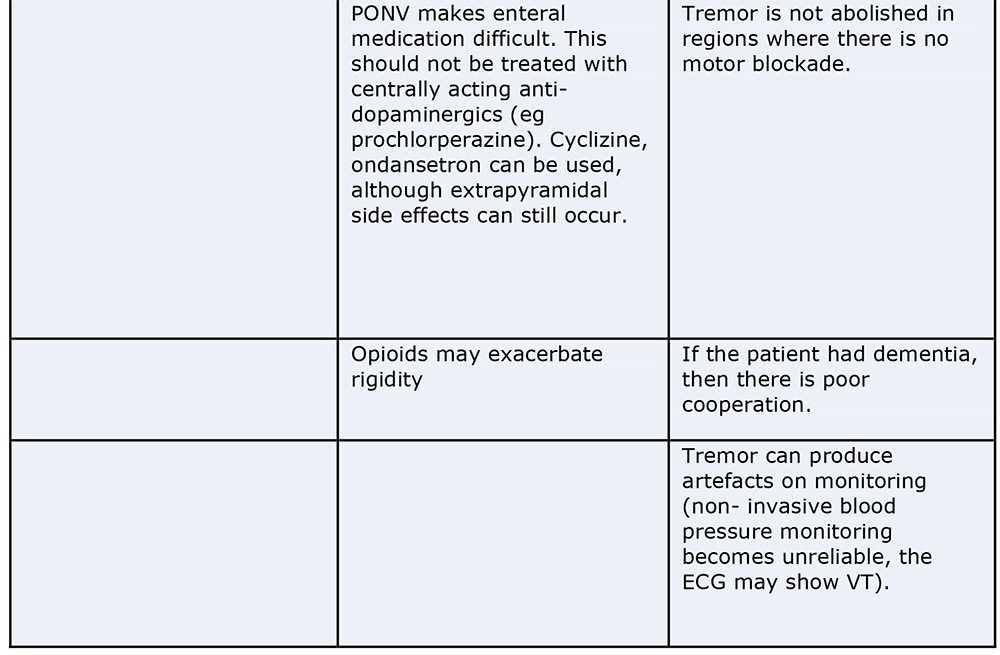
The choice of anaesthesia depends on the type of surgery, and the patient. The advantages and disadvantages of regional versus general anaesthesia (GA) are shown in the table below:
Conclusion
PD is a multi-system disease requiring a multi-disciplinary approach. Good preoperative control of PD, respiratory and musculoskeletal physiotherapy, and good analgesia will reduce the incidence of venous thromboembolism (VTE), pressure area damage, sputum retention and aspiration.
Answers to MCQ’s
- FFFTF
- FFTTT
- TFTTT
- FTTFF – Levodopa and selegiline can be used orally as single agents to treat Parkinson’s disease. Entacapone is used in conjunction with levodopa- DDI. Pethidine should not be used in patients on MAO type B inhibitors.
- TFTTT – rigidity is a feature of PD. PD results in excess saliva/ sialorrhoea. Orthostatic hypotension can be due to PD itself, or due to the effects of dopaminergic or anticholinergic agents used in PD. Respiratory muscle rigidity may result in a restrictive ventilatory defect.
Further Reading:
- Errington DR, Severn AM, Meara J. Parkinsons disease. British Journal of Anaesthesia, CEPD reviews.2002; 2:69-73.
- Nicholson G, Pereira AC, Hall GM. Parkinson’s disease and anaesthesia. British Journal of Anaesthesia. 2002;89:904-16.
- Teasdale A. Parkinson’s disease. Oxford Handbook of Anaesthesia 2nd Edition. Allman KG, Wilson IH. Oxford, 2006.
- Walter B L, Vitek J L. Surgical treatment for Parkinson’s disease. Lancet Neurology.2004;3:719-28
- Krause M, Fogel W, Heck A. Deep Brain Stimulation for the treatment of Parkinson’s Disease: subthalamic nucleus versus globus pallidus internus. J Neurosurg Psychiatry 2001;70:464-470
- Heinonen E H, Myllyla V. Safety of Selegiline in the treatment of Parkinson’s Disease. Drug Safety. 1998;19(1):11-22.



