General Topics
KEY POINTS
- Functional capacity serves as a valuable measure of the body’s ability to effectively respond to and adapt to physiological stress, playing a crucial role in assessing preoperative risk.
- Subjective methods of assessment include determining metabolic equivalents (METs), performing a Duke Activity Status Index (DASI) questionnaire or asking patients about their ability to climb two flights of stairs.
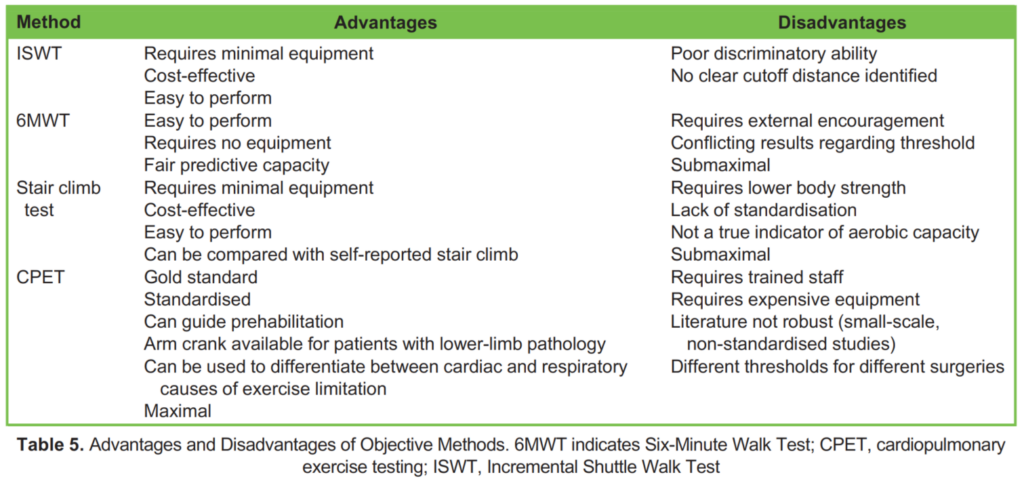
- Objective methods of assessment include the Incremental Shuttle Walk Test (ISWT), the Six Minute Walk Test (6MWT), the Stair Climbing Test or the gold standard Cardiopulmonary Exercise Testing (CPET).
- The literature differs on the sensitivity and specificity of each method and the different thresholds for different surgical populations.
- Currently there is no single, ideal tool to assess functional capacity prior to noncardiac surgery.
INTRODUCTION
Preoperative risk assessment plays a crucial role in identifying patients at increased risk of perioperative morbidity and mortality. It allows clinicians to make informed decisions regarding patient selection for surgery, implement preoperative optimisation strategies, guide intraoperative management, plan for adequate postoperative resources and minimise the risk of avoidable complications. Evaluating functional capacity is an integral component of comprehensive preoperative risk assessment.
Functional capacity is the maximum physical activity that an individual is capable of performing and serves as a valuable measure of the body’s ability to effectively respond and adapt to physiological stress. Patients with good functional capacity have a lower susceptibility to various postoperative complications, including surgical site infections, respiratory issues such as pneumonia, cardiac complications such as myocardial infarction as well as shorter hospital stays and decreased mortality rates.
This tutorial aims to provide an overview of both subjective and objective methods used to assess functional capacity. It will delve into the procedure of each test, highlight their respective advantages and disadvantages, explore their clinical applicability and validity and examine how each test correlates with the gold standard. By covering these aspects, this tutorial aims to enhance understanding and knowledge regarding the perioperative assessment of functional capacity.
Of note, functional capacity assessment may be less accurate in certain populations. In the elderly population, functional capacity does not assess frailty, the presence of dementia or neurocognitive decline. As well, changes in balance and flexibility may make assessment challenging. In the obese population, changes in functional capacity may be related to psychological perceptions (fear or embarrassment) due to social stigmas or obesity-related sarcopenia. In patients with musculoskeletal pathology, physical activity may be limited by pain or immobility and not necessarily due to cardiopulmonary limitations.
SUBJECTIVE METHODS OF ASSESSING FUNCTIONAL CAPACITY
Self-Reported Metabolic Equivalents
A metabolic equivalent (MET) represents the resting oxygen consumption of a 40-year-old, 70-kg man, equivalent to 3.5 mL/kg/min.¹ To assess functional capacity, patients can be asked about their ability to perform various activities of daily living, and the corresponding MET levels can be determined (Table 1).
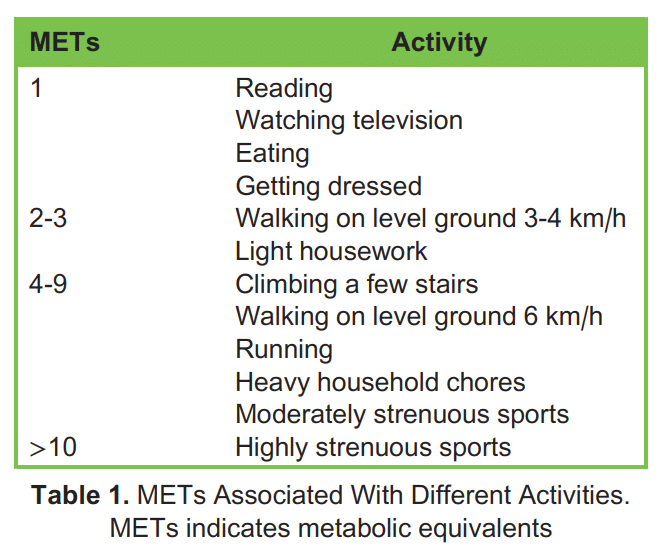
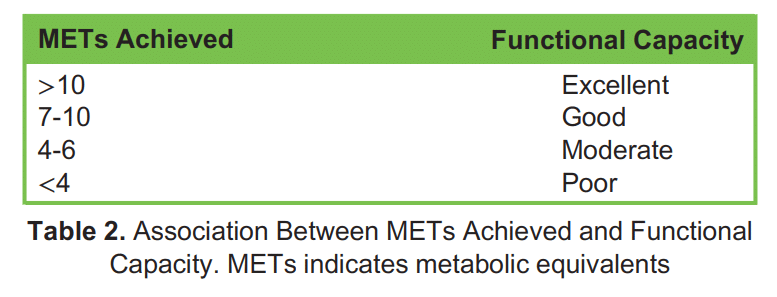
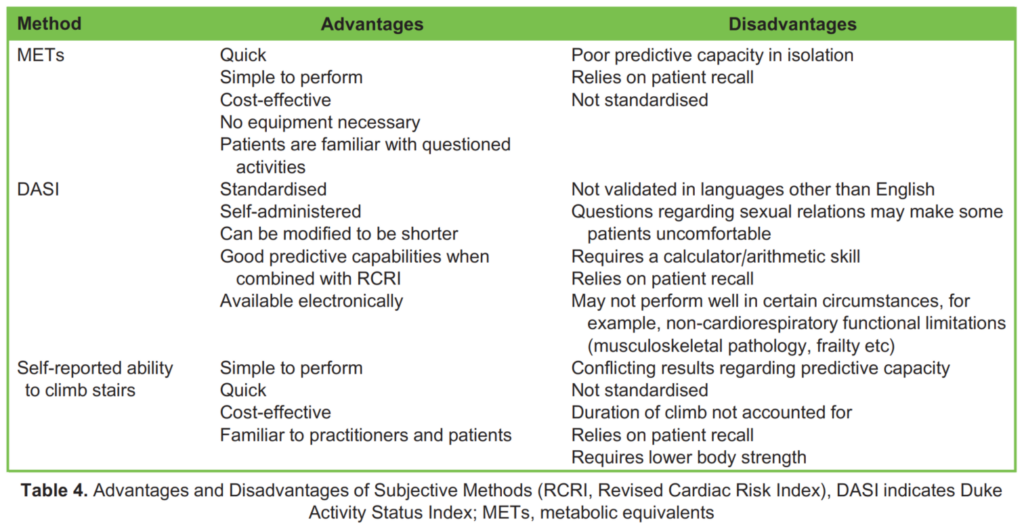
The association between METs achieved and functional capacity is shown in Table 2. Lower MET levels are generally linked to poorer postoperative outcomes.²,³ However, it is important to note that estimating METs solely through a preoperative history of activities of daily living can underestimate the true METs as measured by stress testing.⁴ Therefore, METs should not be solely relied upon but rather assist healthcare practitioners in identifying patients who may require further assessment.
Duke Activity Status Index
To address the limitations of obtaining METs through a general history, a structured, self-administered questionnaire known as the Duke Activity Status Index (DASI) was developed.⁵ The DASI questionnaire consists of 12 activities, ranging from daily living tasks to sports activities, with each activity assigned a weight based on its known energy expenditure (Table 3). The sum of these weights provides a DASI score, which ranges from 0 (equivalent to 2.74 METs, indicating all “no” answers) to 58.2 (approximately 9.89 METs, indicating all “yes” answers). A DASI score below 34 is associated with an increased risk of myocardial infarction, moderate-to-severe complications and new disability following noncardiac surgery.⁶
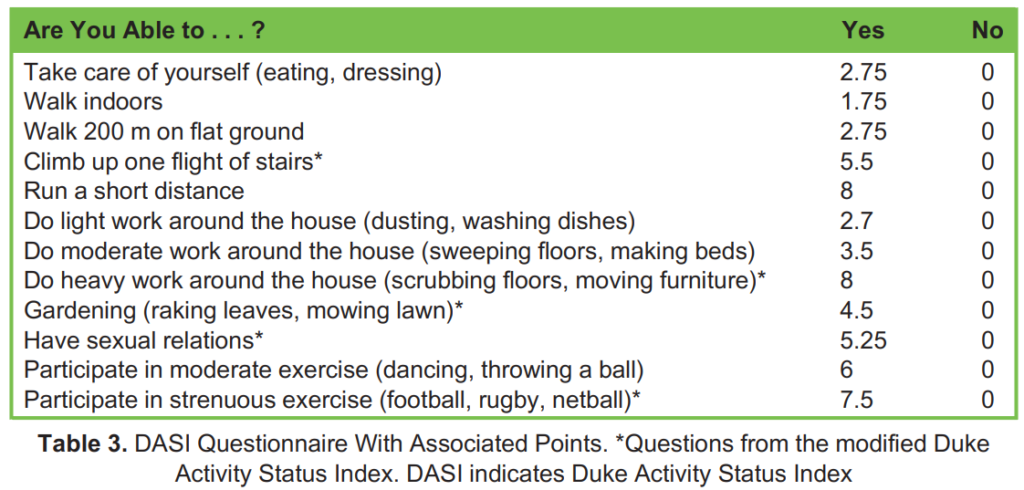
The DASI offers the advantage of being electronically available for completion prior to the preoperative visit, which can streamline the assessment process. In addition, a modified version of the DASI has been developed, comprising only five questions. This shortened version has demonstrated comparable predictive capacity to the original DASI while being more concise and user-friendly.⁷ The correlation between DASI scores and objectively measured methods improves when the questionnaire is administered by an interviewer.⁸ This may be due to patients’ tendency to overestimate their capabilities. The large-scale, multicentre METS study found that the DASI questionnaire performed better than other subjective methods at determining the risk of 30-day myocardial infarction and mortality following abdomino-pelvic and orthopaedic surgeries. The authors also found that when combining the DASI score with the Revised Cardiac Risk Index (RCRI) score, the ability to predict postoperative 30-day mortality, one-year mor- tality and myocardial infarction improved marginally compared with when the RCRI score was used on its own.⁹
Self-Reported Ability to Climb Stairs
Patients are typically asked whether they can climb two flights of stairs without needing to stop. It is worth noting that two flights of stairs generally consist of approximately 44 stairs, with an average step height of 20 cm. However, different institutions may have flights and stairs of varying heights, which could affect standardisation of the test.⁸ The inability to climb two flights of stairs has been associated with increased postoperative complications and mortality. However, there are conflicting data regarding its predictive capacity.¹⁰ The advantages and disadvantages of each subjective method of assessment are detailed below (Table 4).
OBJECTIVE METHODS OF ASSESSING FUNCTIONAL CAPACITY
Indirect Measures
Incremental Shuttle Walk Test
The Incremental Shuttle Walk Test (ISWT) is a maximal exercise test that is considered safe, cost-effective and easy to administer. During the test, the patient walks back and forth between two cones placed 10 m apart, synchronised with auditory beeps that increase in frequency. The test continues until the patient reaches maximal exertion or fails to reach the next cone in time with the beep. If a patient achieves a distance greater than 400 m, further testing is not necessary. However, if the distance achieved is less than 250 m, formal cardiopulmonary exercise testing (CPET) should be considered.¹¹ Notably, in gastro-oesophageal surgery, achieving an ISWT distance of less than 350 m has been associated with reduced long-term survival.¹²
Six-Minute Walk Test
The Six-Minute Walk Test (6MWT) is a submaximal exercise test. During the test, the patient walks at their own comfortable pace for a duration of six minutes, and the total distance covered is measured. An international, multicentre trial found that for every 100-m decrease in the distance achieved on the 6MWT, there was a 1.32-fold increase in the odds of developing postoperative complications following elective noncardiac surgery.¹³ Different studies have found varying threshold distances for identifying high-risk patients, and there are conflicting results regarding the predictive capacity of the 6MWT.¹¹,¹⁴,¹⁵
Stair-Climbing Test
The stair-climbing test is a functional exercise test that is relatively simple to perform. There are two commonly described methods for conducting this test:
- The patient climbs up two flights of stairs as quickly as they can, ensuring safety and without experiencing any limiting symptoms. The time taken to complete the task is recorded.
- The patient climbs up as many flights of stairs as they can until they are unable to continue.
In patients undergoing abdominal surgery, a 12-stair climb duration exceeding 26.5 seconds was associated with a higher risk of postoperative complications, while individuals who completed the stair climb in 15 seconds or less had no postoperative complications.¹⁶ However, the stair-climbing test lacks standardisation in the literature regarding the methods of performance, and it requires sufficient lower body strength to perform. In addition, it may not predict the aerobic capacity necessary to survive the stress response associated with major noncardiac surgery.¹⁷
Direct Measures
Cardiopulmonary Exercise Testing
Cardiopulmonary exercise testing (CPET) is a non-invasive, dynamic and standardised maximal exercise test. Its utilisation, however, is limited by the requirement for expensive equipment and trained personnel. During CPET, the patient undergoes an incremental exercise test with breath-by-breath gas analysis until maximal exercise capacity is reached. The literature surrounding CPET is characterised by small-scale cohort studies and a lack of standardisation.¹⁸ Despite this, it is still considered the gold standard in determining aerobic fitness.¹⁹
The anaerobic threshold (AT), a value determined during CPET, is the exertion level above which lactate begins to increase during incremental exercise. It indicates increased glycolysis and can sometimes be referred to as the lactate threshold. It is an objective value that cannot be affected by the patient’s effort or choice.²⁰ A value <11 mL/kg/min is associated with an increased risk of morbidity and mortality following noncardiopulmonary surgical procedures.²¹,²² Additional values such as the oxygen consumption at peak exercise (VO₂ peak) and ventilatory equivalents (VE/VCO₂) are also used to identify high-risk patients, although specific thresholds may vary depending on the type of surgery.
Notable advantages of CPET are that it can be used to facilitate the implementation of prehabilitation programs aimed at improving a patient’s functional capacity prior to major surgery. As well, an arm crank is available for patients with lower-limb pathology. For more detailed information on CPET, please refer to ATOTW 217 and 473. The advantages and disadvantages of each objective method of assessment are detailed below (Table 5).
VO₂ Peak Equivalents
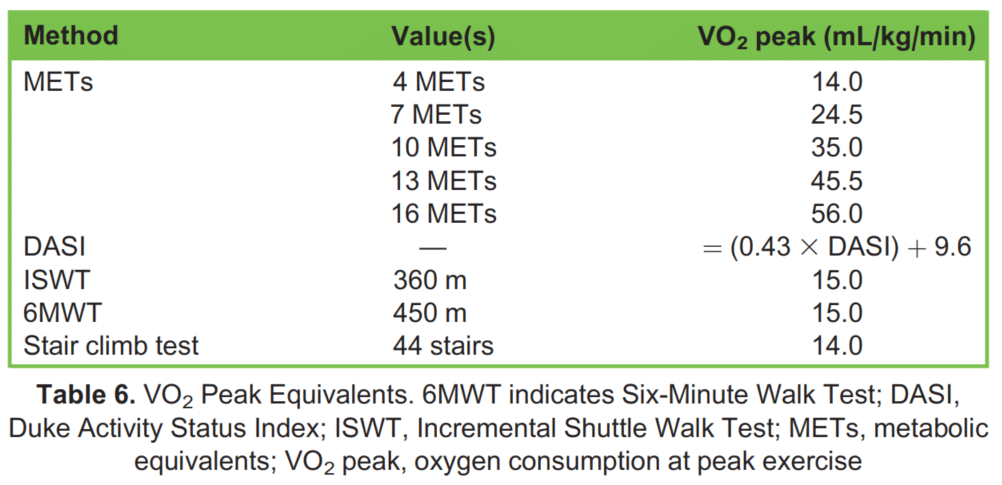
VO₂ peak is a crucial value derived from CPET, representing a patient’s maximum oxygen uptake during peak exercise. VO₂ peak is predictive of postoperative complications such as pulmonary complications, wound infections and unintended admissions to the intensive care unit. Generally, a VO₂ peak value below 15 mL/kg/min is associated with poorer postoperative outcomes.⁸,¹¹ Table 6 illustrates the correlation between each method of functional capacity assessment and VO₂ peak. While the conversions provided in the table are not precise and may not fully capture the increased perioperative morbidity, they offer an estimation for clinicians who do not have access to CPET.
CONCLUSION
It is important to acknowledge that there is currently no flawless method for assessing functional capacity. The information obtained through the aforementioned assessment methods should be carefully analysed in conjunction with other factors such as age, comorbidities, urgency and type of surgery, validated risk scores and biomarkers. This comprehensive evaluation allows for a more accurate quantification of risk and enables shared decision making in the context of preoperative planning.
REFERENCES
- Byrne NM, Hills AP, Hunter GR, Weinsier RL, Schutz Y. Metabolic equivalent: one size does not fit all. J Appl Physiol. 2005;99:1112-1119.
- Van Beijsterveld CA, Bongers BC, Den Dulk M, Van Kuijk SMJ, Dejong KCH, Van Meeteren NLU. The association between preoperative physical functioning and short-term postoperative outcomes: a cohort study of patients undergoing elective hepatic resection. HPB (Oxford). 2019;21:1362-1370.
- Shea C, Khawaja A, Sofi K, Nabi G. Association of metabolic equivalent of task (MET) score in length of stay in hospital fol- lowing radical cystectomy with urinary diversion: a multi-institutional study. Int Urol Nephrol. 2021;53:1-6.
- Weinstein AS, Sigurdsson MI, Bader AM. Comparison of preoperative assessment of patient’s metabolic equivalents (METs) estimated from history versus measured by exercise cardiac stress testing. Anesthesiol Res Pract. 2018;2018:5912726.
- Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (The Duke Activity Status Index). Am J Cardiol. 1989;64(10):651-654.
- Wijeysundera DN, Beattie WS, Hillis GS, et al. Integration of the Duke Activity Status Index into preoperative risk evalua- tion: a multicentre prospective cohort study. Br J Anaesth. 2020;124(3):261-270.
- Riedel B, Li MHG, Lee CHA, et al. A simplified (modified) Duke Activity Status Index (M-DASI) to characterise functional capacity: a secondary analysis of the measurement of exercise tolerance before surgery (METS) study. Br J Anaesth. 2021;126(1):181-190.
- Silvapulle E, Darvall J. Subjective methods for preoperative assessment of functional capacity. Br J Anaesth. 2022;22(7): 249-257.
- Wijeysundera DN, Pearse RM, Shulman MA, et al. Assessment of functional capacity before major non-cardiac surgery: an international, prospective cohort study. Lancet. 2018;391(10140):2631-2640.
- Girish M, Trayner E Jr, Dammann O, Pinto-Plata V, Celli B. Symptom-limited stair climbing as a predictor of postoperative cardiopulmonary complications after high-risk surgery. Chest. 2001;120(4):1147-1151.
- Silvapulle E, Darvall J. Objective methods for preoperative assessment of functional capacity. Br J Anaesth. 2022;22(8):312-320.
- Whibley J, Peters CJ, Halliday LJ, Chaudry AM, Allum WH. Poor performance in incremental shuttle walk and cardiopulmo- nary exercise testing predicts poor overall survival for patients undergoing esophago-gastric resection. Eur J Surg Oncol. 2018;44(5):594-599.
- Ramos RJ, Ladha KS, Cuthbertson BH, et al. Association of six-minute walk test distance with postoperative complications in non-cardiac surgery: a secondary analysis of a multicentre prospective cohort study. Can J Anaesth. 2021;68(4):514-529.
- Sathyaprasad SL, Thomas M, Philip FA, Krishna KJ. Performance in 6-min walk test in prediction of post-operative pulmonary complication in major oncosurgeries: a prospective observational study. Indian J Anaesth. 2020;64:55-61.
- Sinclair RCF, Batterham AM, Davies S, Cawthorn L, Danjoux GR. Validity of the 6 min walk test in prediction of the anaero- bic threshold before major non-cardiac surgery. Br J Anaesth. 2012;108:30-35.
- Baker S, Waldrop MG, Swords J, et al. Timed stair-climbing as a surrogate marker for sarcopenia measurements in predicting surgical outcomes. J Gastrointest Surg. 2019;23(12):2459-2465.
- Biccard BM. Relationship between the inability to climb two flights of stairs and outcome after major non-cardiac surgery: implications for the pre-operative assessment of functional capacity. Anaesthesia. 2005;60(6):588-593.
- Biccard BM. Improving the evidence-base for preoperative cardiopulmonary exercise testing. Br J Anaesth. 2018;120:419-421.
- Pritchard A, Burns P, Correia J, et al. ARTP statement on cardiopulmonary exercise testing 2021. BMJ Open Resp Res. 2021;1:8.
- Levett DZH, Jack S, Swart M, et al. Perioperative cardiopulmonary exercise testing (CPET): consensus clinical guidelines on indications, organization, conduct, and physiological interpretation. Br J Anaesth. 2018;120:484-500.
- Moran J, Wilson F, Guinan E, McCormick P, Hussey J, Moriarty J. Role of cardiopulmonary exercise testing as a risk-assessment method in patients undergoing intra-abdominal surgery: a systematic review. Br J Anaesth. 2016;116(2):177-191.
- Young EL, Karthikesalingam A, Huddart S, et al. A systematic review of the role of cardiopulmonary exercise testing in vascular surgery. Eur J Vasc Endovasc Surg. 2012;44(1):64-71.



