Paediatric Anaesthesia
KEY POINTS
- Understanding the difference in anatomy, physiology and pharmacology between adults and children is essential when performing paediatric regional anaesthesia (PRA).
- PRA techniques help ensure optimal analgesia, early ambulation and earlier discharge from hospital.
- PRA can be performed safely under general anaesthesia or deep sedation.
- Ultrasound guidance reduces the risk of inadvertent vascular, nerve or organ injury.
- To avoid life-threatening local anaesthetic systemic toxicity, the maximum recommended dose of local anaesthetic should be calculated prior to administration.
INTRODUCTION
Paediatric regional anaesthesia (PRA) helps to ensure optimal analgesia. It is opioid sparing and has beneficial effects on the autonomic, metabolic and immunological systems.1 Regional anaesthesia is a useful adjunct that can reduce the dose of general anaesthetic agents required, and in some cases may be used as a sole anaesthetic technique or with minimal sedation (for example, spinal anaesthesia).1,2 An appreciation of the differences in the anatomy, physiology, pharmacology and controversies associated with regional anaesthesia in children compared with adults is required prior to performing PRA to ensure it is performed safely and effectively.
ANATOMICAL DIFFERENCES
Central Nervous System
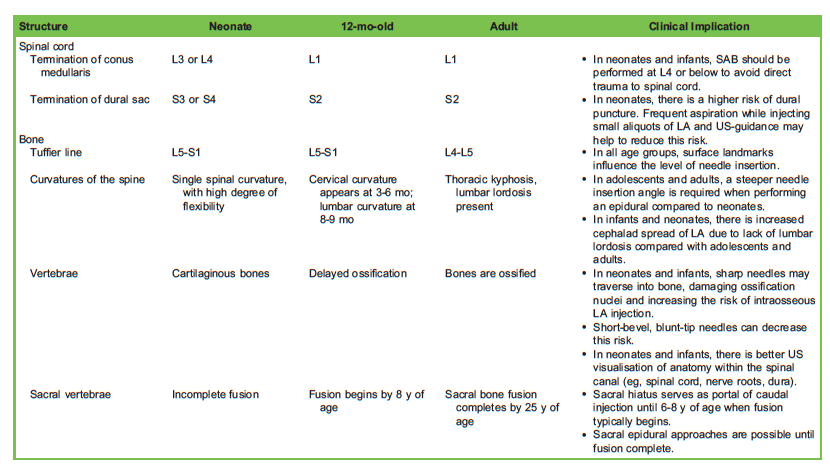
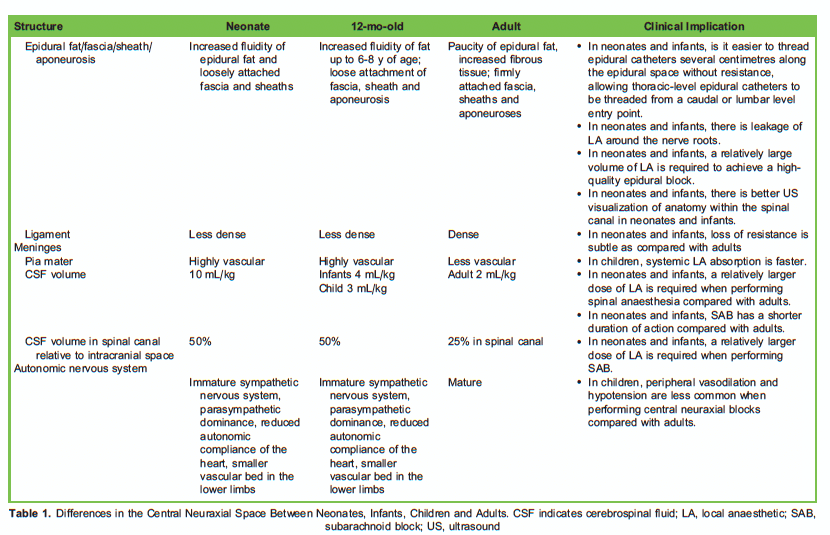
During normal development, the rate of growth of the vertebral column exceeds that of the spinal cord. This has clinically significant implications for the relationship between surface landmarks and anatomy when performing central neuraxial blocks in paediatric patients. The changes in the central nervous system with increasing age are outlined in Table 1.2-4
Peripheral Nervous System
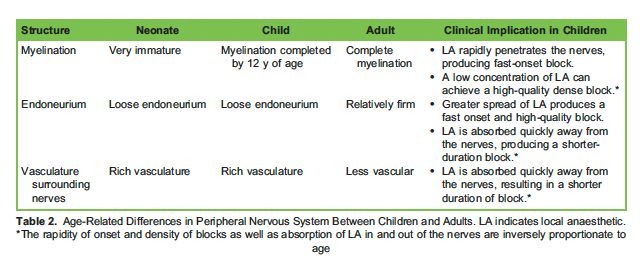
The differences between children and adults are outlined in Table 2.2,5
LOCAL ANAESTHETIC CHOICE
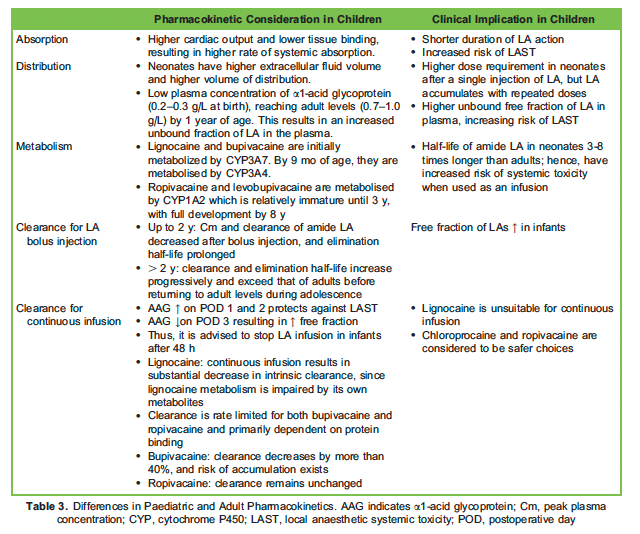
Amide local anaesthetics (LAs) are frequently used in PRA. Ropivacaine and levobupivacaine are considered less cardiotoxic than bupivacaine.6 Ester LAs, such as chloroprocaine, are metabolized efficiently by plasma cholinesterases and are considered safer than amide LAs.6,7 Important differences in the pharmacokinetics in children are outlined in Table 3.3,8,9
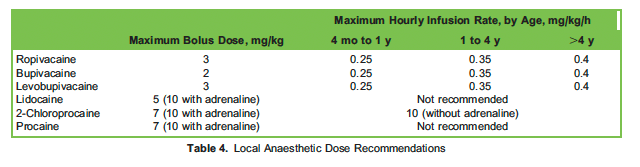
Weight-based calculation of the maximum LA dose is essential in avoiding life-threatening local anaesthetic systemic toxicity (LAST).10Recommended doses are outlined in Table 4.2
ADDITIVES
Currently, there is no strong evidence for the routine use of additives in PRA. However, clonidine (1-2 μg/kg) or dexmedetomidine (1 μg/kg) are popular additives and may prolong analgesia.11 Clonidine can be safely used in central neuraxial blocks. Both clonidine and dexmedetomidine are systemically absorbed and will contribute to postoperative sedation. Clonidine and dexmedetomidine are usually avoided in preterm babies and in infants less than 6 months old due to systemic absorption and prolonged sedation. Adrenaline is not recommended due to the risk of spinal cord ischaemia.12
PERIPHERAL NERVE CATHETERS
Peripheral nerve catheters (PNCs) allow continuous analgesia and should be considered for any child who has (or is anticipated to have) significant acute pain, such as postoperative pain, ischemic pain or amputation pain.2 PNCs reduce opioid requirements and subsequently minimize the risk of opioid-related adverse effects, such as nausea, vomiting, constipation and respiratory depression.
Compared with a single injection regional block, continuous catheter techniques allow the following:
- Prolonged duration of analgesia
- Reduced opioid requirement and opioid-associated adverse effects
- Earlier ambulation2
- Shorter hospital stay2
A PNC can be left in situ for up to 7 days; however, each additional day beyond the fourth day increases the risk of catheter-related infection.13 When deciding upon the duration of catheter use, the analgesic benefits should be weighed against the risk of infection.
Complications specifically related to PNC include the following:
- Catheter equipment failure, including dislodgement, migration, blockage, leakage, disconnection
- Skin reactions resulting from dressings
- Risks associated with single injection techniques (eg, nerve injury, failed block, LAST)
EQUIPMENT
Age-appropriate equipment should be used to maximize the likelihood of block success and minimize the risk of inadvertent vascular or organ injury. Note also the following:
- Use ultrasound (US) guidance to allow accurate catheter placement and reduce the risk of inadvertent vascular or organ injury.14 This is particularly important in children because their nerves are more superficial and adjacent major organ and vascular structures are in close proximity.
- When selecting an appropriate needle, consider the depth of the intended block to be performed and the size of the patient. Consider using a smaller gauge to minimize local tissue trauma. A shorter needle length will maximize needle control during block placement.
- Use a short bevel or Touhy needle; it is associated with less risk of direct nerve injury compared with a sharp, long-bevelled needle.
- To minimize the risk of catheter dislodgement, secure the catheter carefully and consider tunnelling it.
CONTROVERSIES
Awake Versus General Anaesthesia
In adult patients, regional anaesthesia performed awake or under light sedation allows early detection of LAST and reduced risk of intraneural injection. However, in children, performing a regional block awake or with minimal sedation may result in child distress and movement during block placement. Furthermore, a frightened child is unlikely to report symptoms of LAST. The American and European Societies of Regional Anaesthesia Joint Committee Statement recommends that PRA performed under general anaesthesia or deep sedation has an acceptable safety profile and is considered to be the standard of care.15
Compartment Syndrome
Compartment syndrome (CS) is caused by increased pressure inside a fascial compartment resulting in impaired blood flow and, if unrecognized, may result in muscle ischaemia and myonecrosis. One of the early symptoms of CS is pain, and there is concern that PRA could mask this pain. While there is no current evidence that the use of regional analgesia increases the risk of CS or delays its diagnosis,15 caution should be exercised, and we recommend the following for patients at risk of CS:
- Maintain a high index of suspicion and careful monitoring. If CS is suspected, compartment pressures should be urgently assessed.
- Use dilute LA solutions (eg, 1% ropivacaine) because they are less likely to mask ischaemic pain and less likely to produce a motor block.
- Avoid the use of additives because they will increase the density of the sensory and motor block.15
Saline Versus Air
The most common techniques for performing an epidural block are loss of resistance (LOR) to saline, LOR to air or a combination of these techniques.
LOR to air may be associated with a risk of air embolism, incomplete analgesia due to air trapping, nerve root compression, subcutaneousemphysema and pneumocephalus. These risks are heightened in infants and neonates because their epidural space is smaller and the same volume of air would cause more disturbance. The total volume of injected air should not exceed 0.5-1 mL in infants and neonates.
LOR to saline overcomes many of the issues associated with the LOR to air technique; however, the volume of saline injected should still be minimised because this can dilute the LA injected, and a large volume of injectate may cause a transient reduction in cerebral blood flow in smaller infants and neonates.16 Furthermore, it may be more difficult to identify a dural puncture using the LOR saline technique because of the inability to easily differentiate between saline and cerebrospinal fluid.
A combination of air and saline allows for an obvious LOR while minimising the risk of injecting air and minimising the volume of saline injected.15 This technique is also associated with a lower risk of dural puncture than when either saline or air is used alone. There is currently no clear evidence regarding which technique is superior, and any of the above techniques are acceptable provided the injected volume is kept to a minimum.15
Patients With Preexisting Neurologic Conditions
In patients with preexisting neurologic conditions affecting cardiac and respiratory function, PRA may be beneficial in optimising analgesia, minimising opioid-related ventilatory impairment and minimising haemodynamic disturbances related to pain after surgery. However, there is concern that PRA may create new or worsened neurologic deficits, due to the dose-dependent neurotoxicity of LAs.17 Preexisting neurologic disease is not an absolute contraindication to PRA. If PRA is planned, a thorough neurological examination should be documented prior to the procedure. A conservative approach is recommended, and the individual patient’s risks versus benefits should be carefully considered.17
Liposomal Bupivacaine in RA
Studies have revealed no superiority of liposomal bupivacaine over nonliposomal bupivacaine in peripheral nerve blocks. Currently, there is no role for liposomal bupivacaine in paediatric regional analgesia, and more evidence is required to support its use.18
SAFETY
US and Peripheral Nerve Stimulation
US allows visualisation of the needle tip and spread of injected LA, and it minimises the risk of inadvertent injury to nearby vascular or organ structures. Furthermore, the use of US results in faster onset, increases the duration, increases the block density and reduces the LA volume required. There are fewer needle insertions and better user appreciation of the underlying anatomy.2 In children, linear high-frequency probes can be used for most blocks.
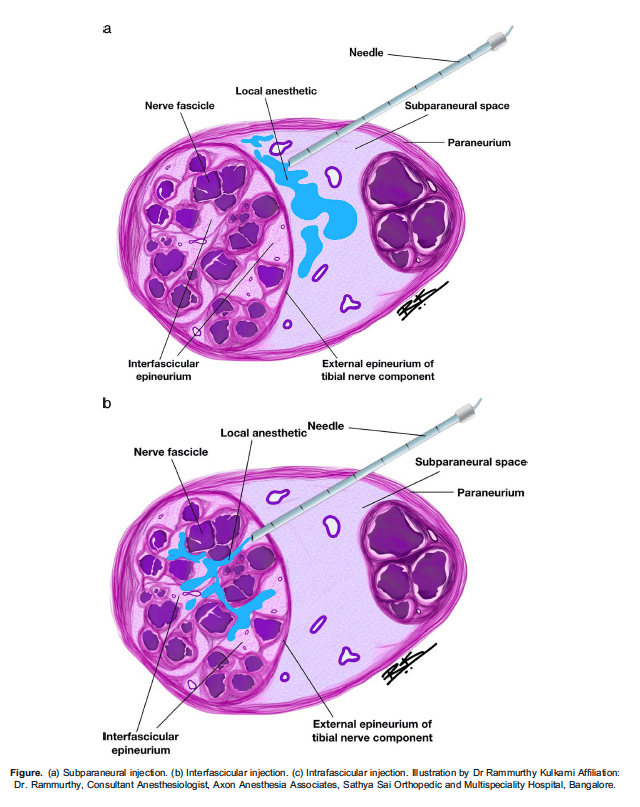
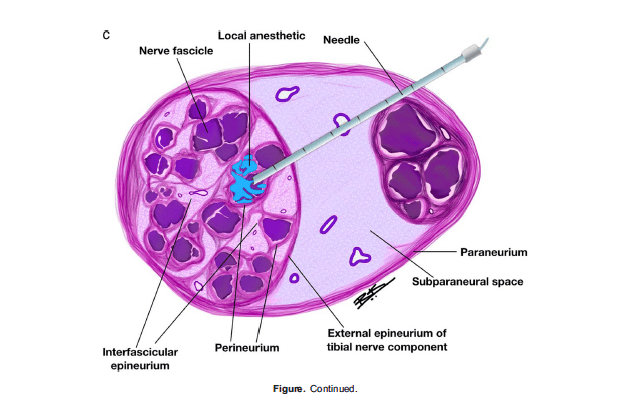
Peripheral nerve stimulation is a useful adjunct when combined with US guidance. The needle position is judged to be adequate when muscle contraction in the desired nerve distribution occurs at 0.5-0.8 mA. If muscle contractions continue to occur at <0.5 mA, the needle should be withdrawn slightly to avoid nerve damage or intraneural injection (Figure a-c). This technique is useful to improve reliability when teaching trainees, for deeper blocks when perfect nerve visualisation may not be possible (such as the lumbar plexus block, anterior sciatic block) and in low-resource settings where US equipment may not be available.2
Test Dosing
A test dose containing LA, adrenaline or both, may be administered to identify inadvertent intravascular needle placement.19 The paediatric test dose is 0.5 μg/kg of adrenaline (or 0.1 mL/kg of LA containing 5 μg/mL adrenalin). Some institutions use 1.5% lidocaine with 1:200 000 adrenaline. A positive test dose is defined as an increase in heart rate (>10 beats per minute), increase in systolic blood pressure (>15 mm Hg) or 25% change in T-wave amplitude or ST segment size. However, test doses have a high false-negative rate.19 Other methods of detecting intravascular needle placement include aspiration for blood and observing the LA spread during injection on US. However, there is no absolutely reliable method to detect intravascular needle placement; therefore, we recommend that any injection of LA is performed slowly with intermittent aspiration while observing the electrocardiographic morphology.19
Aseptic Precautions
Regional blocks must be performed under aseptic conditions to minimize the risk of infection. For children younger than 2 months, chlorhexidine(2% or 1%) can cause chemical burns, so alcohol is preferred.20 In older children, 2% chlorhexidine with 70% alcohol is recommended.
Local Anaesthetic Systemic Toxicity
When PRA is performed under general anaesthesia or deep sedation, the earliest signs of LAST are cardiovascular including peaked T waves and dysrhythmias. Infants <6 months old are at highest risk of LAST due to unrecognized intravascular injection, rapid absorption, distribution of LA and decreased levels of α1-acid glycoprotein.2 All providers must be familiar with current LAST management guidelines, and weight-based dosing must be followed.
ENHANCED RECOVERY AFTER SURGERY
Enhanced recovery after surgery (ERAS) protocols are multidisciplinary, multimodal, evidence-based pathways designed to optimize perioperative medical care and facilitate early recovery.2 Regional anaesthesia is an important element of ERAS because it allows optimal analgesia, reduces opioid requirements and facilitates earlier return of bowel function and ambulation.2
SUMMARY
REFERENCES
- Bosenberg Benefits of regional anaesthesia in children. Paediatr Anaesth. 2012;22:10-18.
- Suresh S, Lonnqvist PA. Regional anesthesia in children. In: Gropper MA, ed. Miller’s Anesthesia. 9th ed. Philadelphia: Elsevier; 2020:2368-2419.
- Tetzlaff JE. Cousins and Bridenbaugh’s neural blockade in clinical anesthesia and pain medicine. Mayo Clin Proc. 2010; 85:51.
- Jain D, Hussain SY, Ayub Comparative evaluation of landmark technique and ultrasound-guided caudal epidural injection in paediatric population: a systematic review and meta-analysis. Paediatr Anaesth. 2022;32:35-42.
- Tsui B, Suresh Pediatric Atlas of Ultrasound-And Nerve Stimulation-Guided Regional Anesthesia. New York: Springer; 2016.
- Boretsky A review of regional anaesthesia in infants. Paediatr Drugs. 2019;21:439-449.
- Graf BM, Abraham I, Eberbach N, Kunst G, Stowe DF, Martin Differences in cardiotoxicity of bupivacaine and ropivacaine are the result of physicochemical and stereoselective properties. Anesthesiology. 2002;96:1427-1433.
- Cousins M, Bridenbaugh P, Carr D. Cousins and Bridenbaugh’s Neural Blockade. 4th ed. Philadelphia: Wolters Kluwer Health; 2011.
- Ramamurthi RJ, Krane Local anesthetic pharmacology in pediatric anesthesia. Tech Reg Anesth Pain Manag. 2007;11:229-234.
- Neal JM, Neal EJ, Weinberg American Society of Regional Anaesthesia and Pain Medicine local anaesthetic systemic toxicity checklist: 2020 version. Reg Anaesth Pain Med. 2021;46:81-82.
- Bosenberg Adjuvants in pediatric regional anesthesia. Pain Manage. 2012;2:479-486.
- Meyer MJ, Krane EJ, Goldschneider KR, et Neurological complications associated with epidural analgesia in children: a report of 4 cases of ambiguous etiologies. Anaesth Analg. 2012;115(6):1365-1370.
- Bomberg H, Bayer I, Wagenpfeil S, et al. Prolonged catheter use and infection in regional anesthesia: a retrospective registry analysis. Anesthesiology. 2018;128:764-773.
- Barrington MJ, Kluger R. Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth Pain Med. 2013;38:289-299.
- Ivani G, Suresh S, Ecoffey C, et al. The European Society of Regional Anaesthesia and Pain Therapy and the American Society of RegionalAnesthesia and Pain Medicine Joint Committee Practice Advisory on Controversial Topics in Pediatric Regional Anesthesia. Reg Anesth Pain Med. 2015;40:526-532.
- Park J, Hong J, Kim J, Yi S. The effect of different posture on normal saline injection in optic nerve sheath diameter in thoracic epidural anesthesia. Pain Physician. 2020;23(6):573-579.
- Cung S, Ritz ML, Masaracchia Regional anesthesia in pediatric patients with preexisting neurological disease. Pediatr Anesth. 2021:31:522-530.
- Hussain N, Brull R, Sheehy B, et Perineural liposomal bupivacaine is not superior to nonliposomal bupivacaine for peripheral nerve block analgesia. Anesthesiology. 2021;134(2):147-164.
- Tobias Caudal epidural block: a review of test dosing and recognition of systemic injection in children. Anaesth Analg. 2001;93:1156-1161.
- Chlorhexidine gluconate solution product Accessed May 12, 2021. https://dailymed.nlm.nih.gov/dailymed/fda/ fdaDrugXsl.cfm?setid=76cfedb3-25ed-4c12-8ebc-b57f029fedaa&type=display



