Basic Sciences
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation. Please answer True or False:
- Regarding the pharmacology of remifentanil:
a. The pharmacodynamics are more closely related to lean body weight than to actual body weight
b. The dose of remifentanil needs to be altered in patients with a low creatinine clearance
c. Post-operative shivering is less common with remifentanil compared to other opioids
d. Remifentanil has a half-life of approximately 3 minutes
e. It should be avoided in patients with suxamethonium apnoea as it is also broken down by plasma esterases - Regarding target controlled infusions (TCI) of remifentanil and Total Intravenous Anaesthesia (TIVA):
a. The Marsh model is used to predict target organ concentrations of remifentanil
b. The only patient specific data required for the TCI pump are height, weight and gender
c. Remifentanil use is associated with a lower propofol requirement during TIVA
d. The effect site concentration of remifentanil should be kept between 2-12micrograms per ml (mcg.ml-1) for intraoperative analgesic maintenance
e. The bolus dose of remifentanil delivered is three to four times greater with plasma-site targeting (Cpt) compared to effect-site targeting (Cet) - Clinical applications of remifentanil include:
a. Intubation without muscle relaxants
b. Post-op patient controlled analgesia (PCA) on the ward
c. Burns dressing changes
d. Analgesia/sedation in the ICU
e. Labour PCA
Key Points
- Remifentanil is a versatile drug that can be used in various anaesthetic and critical care situations
- It has an ultrafast offset and short contextsensitive half-life, making it an ideal agent for analgo-sedation in ICU
- It can be used effectively for awake fibre-optic intubation and conscious sedation
- When epidural is not possible, remifentanil patient-controlled analgesia can be used in obstetric units that are set up for its use
- Using target controlled infusions and avoiding boluses will help to avoid significant cardiovascular and respiratory side effects of remifentanil
INTRODUCTION
Remifentanil is a pure μ-opioid receptor agonist. Introduced in the early 1990s, its rapid onset and offset coupled with its synergistic effects with other general anaesthetic agents make it an ideal option for anaesthesia and conscious sedation. Its repertoire is ever growing as anaesthetists and intensivists across the world push the boundaries of its use. This tutorial will cover the basic pharmacology of remifentanil, common and novel uses in clinical practice and key safety considerations.
BASIC PHARMACOLOGY
The structure of remifentanil, like alfentanil and sufentanil, is based on its parent drug fentanyl (Figure 1). The crucial difference is the addition of an ester group (highlighted) allowing it to be rapidly metabolized by non-specific plasma and tissue esterases. This gives rise to its characteristic ultra-fast offset and allows for rapid titration.
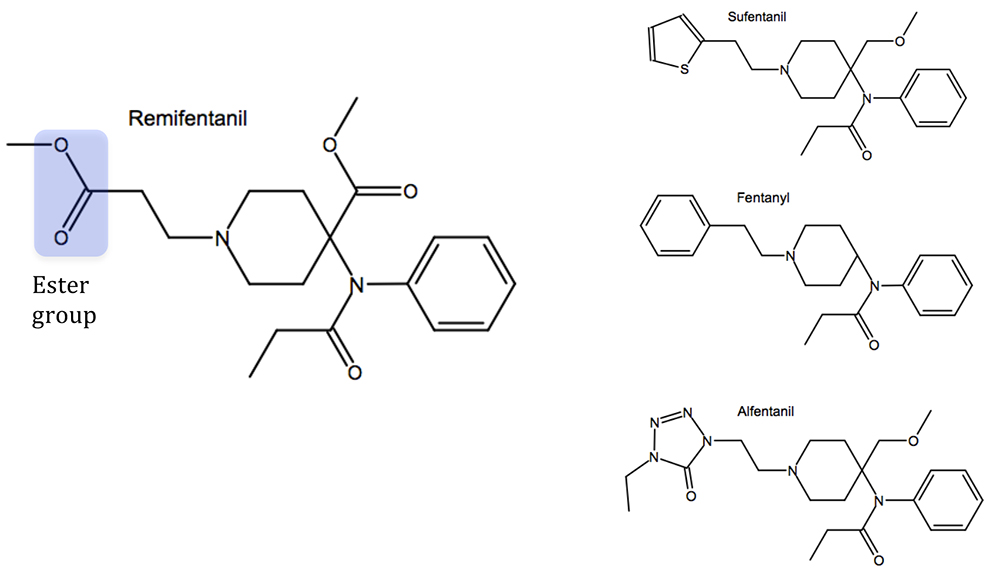
Figure 1. Structure of remifentanil compared to other opioids
Despite being broken down by esterases, remifentanil can be used safely in patients with pseudocholinesterase deficiency1. Its major metabolite, remifentanil acid, undergoes renal excretion and accumulates in patients with reduced renal function1,2. Despite this, the dosing of remifentanil does not need to be adjusted for renal dysfunction as remifentanil acid is almost entirely inactive1,2.
Remifentanil’s side effect profile is similar to that of other opioids (Figure 2).
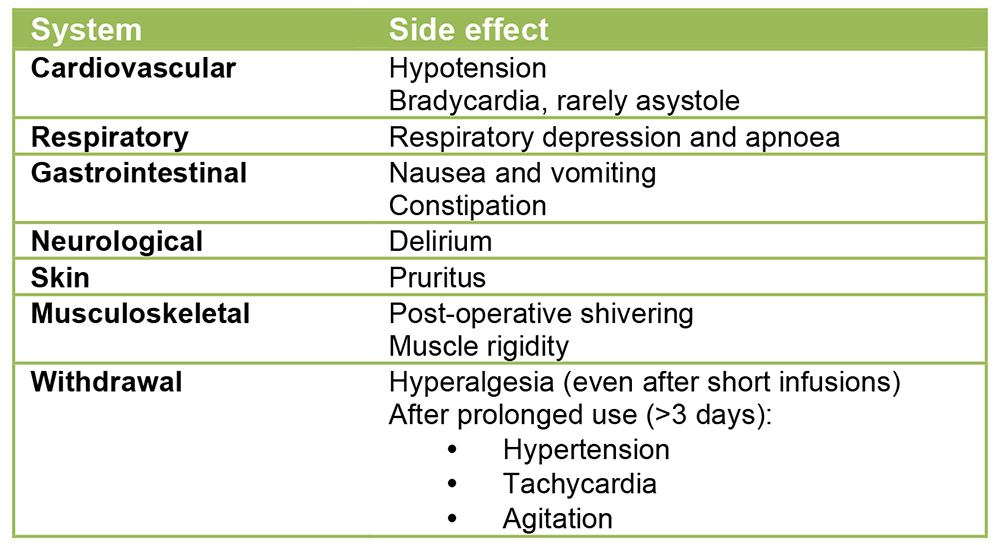
Figure 2. Side effects of remifentanil
When comparing remifentanil to other short acting opioids (fentanyl, alfentanil and sufentanil), it is associated with deeper anaesthesia and analgesia intra-operatively3. This manifests as a lower blood pressure and heart rate3. Higher doses of remifentanil are associated with an increased risk of hypotension and bradycardia as well as apnoea3. It is prudent to have vasopressors and anticholinergics to hand when using remifentanil.
High intra-operative doses of remifentanil have been associated with post-operative hyperalgesia4, although this may be due in-part to inadequate provision of post op-analgesia. As a guide, morphine (0.15–0.3mg.kg-1) or alternative, should be given at least 30 minutes before stopping remifentanil to allow it time to reach peak effect. Despite the occasional use of rescue analgesia, naloxone is less likely to be needed following intraoperative remifentanil use3. The incidence of nausea and vomiting remains similar to other short acting opioids, however this appears to be less common when using remifentanil as part of a Total Intravenous Anaesthesia (TIVA) technique. Post-operative shivering is twice as likely to occur with remifentanil3.
The pharmacokinetics of remifentanil are more closely associated with lean body weight (LBW) rather than actual body weight (ABW)1. Although obese patients do require a larger dose than their LBW would suggest, it is far less than their ABW dose; this would put them at risk of cardiovascular depression1.
Minto Model
Target controlled infusion (TCI) pumps adjust the rate of a drug infusion to achieve a steady effect site concentration taking into account the known pharmacokinetics of the drug and physical characteristics of the patient. The Minto model, named after one of its developers, Dr. Charles Minto, is a model for predicting the concentration of remifentanil in plasma and the effect site. While more accurate models exist (the Minto model can over-predict by as much as 15%5) its versatility and wider body of experience have led to it being the most widely used model.
The Minto model is a three-compartment model programmed to target either effect site (Cet) or plasma site (Cpt). The Cet rate constant (keo) and loss-of-consciousness effect have been derived from electroencephalogram (EEG) parameters. The initial bolus dose delivered in Cet mode is 3-4x greater when compared to Cpt; this may be associated with a greater incidence of adverse effects (e.g. chest wall rigidity, bradycardia, apnoea). Often this can be attenuated by an incremental dosing approach to the desired Cet and the bradycardia can be managed with prophylactic glycopyrrolate. It is advisable that clinicians unfamiliar with the use of remifentanil TCI use Cpt in preference to Cet.
TCIs, such as the Minto model, give users an advantage over those who use “mcg.kg-1.min-1” as they take a number of patient characteristics, not just ABW, to predict the pharmacokinetics of remifentanil in an individual patient. The Minto model requires input of patient sex, age, weight (kg) and height (cm); these are used to calculate LBW. It is not applicable to the majority of paediatric patients with an age cut off of greater than 12 years and a minimum weight of 30kg, and unfortunately there aren’t currently any widely available models for use in children; we suspect this will change in the future. Age is an important determinant, as the pharmacokinetics of remifentanil vary greatly with age; for example 85 year olds have a 25% reduction in the volume of distribution of remifentanil and two-thirds the clearance rate compared to 20 year olds6. Special care must be exercised in frail, elderly patients in order to limit cardiovascular and respiratory complications. This is more easily achieved using a TCI rather than the simpler mcg.kg-1.min-1 technique.
Below is a graph and table (figure 3) of remifentanil blood concentrations, as predicted by the Minto model, plotted against various infusion rates in a 70kg, 170 cm, 40-year-old male.
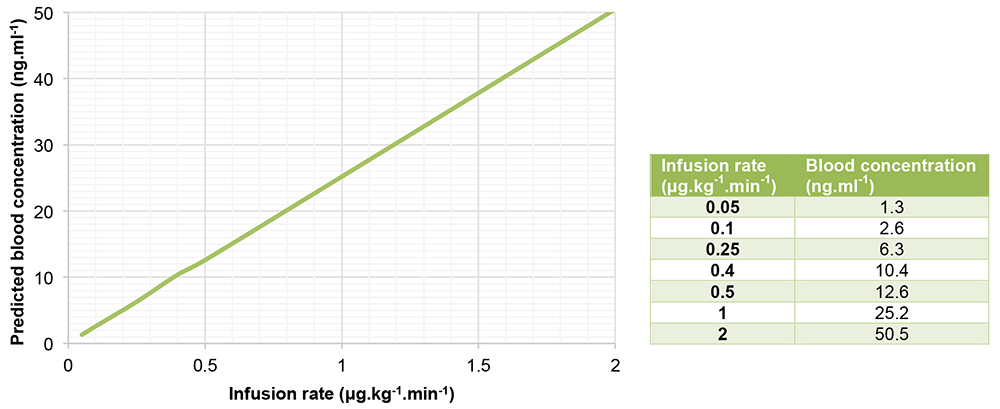
Figure 3
CLINICAL APPLICATIONS
General Anaesthesia
Use of remifentanil during general anaesthesia usually requires a Cet of 3-10 ng.ml-1 or about “0.1-0.3 μg.kg-1.min-1”. Bispectral index (BIS) monitoring offers an alternative means of titration i.e. if the BIS is outside acceptable ranges (e.g.<40 or >55) the remifentanil can be titrated up or down by 0.05ng.ml-1.
Due to its potent respiratory depressant effects, achieving spontaneous ventilation with TCI remifentanil can be challenging especially with higher rates. If using a TIVA technique combining remifentanil and propofol it is advisable to use higher propofol rates (Cet 4-6μg.ml-1) with lower remifentanil rates (Cet 2.5ng.ml-1) in order to maintain spontaneous ventilation under general anaesthesia. Once spontaneous breathing is achieved, it may then be possible to titrate up the remifentanil in small increments (i.e. 0.05ng.ml-1) until adequate analgesia is reached. In this instance, monitoring of respiratory rate may help to guide analgesia with rates of 10-15 breaths per minute suggesting adequate analgesic control.
Remifentanil is an excellent choice for TIVA; it is safe in malignant hyperthermia and reduces the need for higher doses of propofol due to a synergistic interaction between the two drugs7. Dosage of remifentanil depends on clinical experience, user preference and patient/operative factors. As a rough guide, the propofol Cet should be kept at 2-4μg.ml-1 to ensure anaesthesia with remifentanil titrated between 6-12ng.ml-1 (low propofol, high remifentanil) or propofol concentration 5-6ug.ml-1 with remifentanil 0.5-3ng.ml-1 (high propofol, low remifentanil) for less noxious procedures or in patients where spontaneous breathing is desired7. Generally speaking, a low propofol, high remifentanil technique is associated with a more rapid wake-up time8. Higher concentrations of remifentanil will be needed in younger, fitter, more muscular patients; where surgery is more painful and in patients with a history of opioid tolerance, for example in those with a history of chronic pain or intravenous drug use. With higher concentrations of remifentanil, be mindful that there is a greater potential for adverse cardiovascular and respiratory effects.
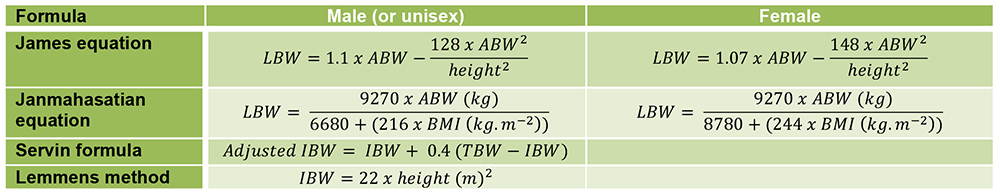
One note of caution: it is important that the IBW weight used in the Minto model at the start of the case closely reflects that of the patient and is accurate, particularly if they are morbidly obese. IBW is accurately calculated by the TCI pump using the James equation up to BMI 42 in men and 37 in women, after which a paradoxical decrease in IBW occurs. If the estimated IBW weight used is too low, this can produce a confusing situation where a patient appears to require much higher doses of remifentanil than would be expected for a given BIS value and stage of surgery. If this error occurs, the weight cannot be changed intra-operatively without negating the whole model, so it is important to estimate IBW weight accurately from the start. This is a controversial area, but the Janmahasatian equation may offer a more accurate estimate for IBW in the morbidly obese, but it is more cumbersome to use8. Some clinicians advocate the use of the Servin formula or Lemmens method which gives an acceptable adjusted IBW compromise, one that is between ABW (which may be too high) and IBW (which may be too low)9,10. These formulae are often used in propofol TCI models but can also be used with remifentanil9,10. It is also important, where possible, to ensure that a patient has a recent, accurate ABW measured preoperatively, rather than relying on any estimated weights given, which can be notoriously inaccurate.
Summary of the various formulae used to calculate IBW or LBW (for reference) (all weights in kg) 8,9,10:
Remifentanil has a relatively short context-sensitive half-time of only 3 to 4 minutes11. Clinically it takes about 6-12 minutes before a patient will resume spontaneous ventilation after remifentanil is stopped or reduced to low Cet (approximately 2.5ng.ml-1). Numerous factors will influence this, such as the Cet at the time of turning off the infusion and the presence of other respiratory depressant drugs. It is important to consider these facts when timing wake up to ensure patients breathe and emerge from anaesthesia in a timely and appropriate manner at the end of surgery. This predictable property makes remifentanil useful for longer operations, for patients in whom rapid wake-up times are desirable e.g. post-neurosurgery, in obese patients, or when post-operative respiratory depression needs to be avoided, for example obstructive sleep apnoea.
Remifentanil has been described as part of a modified rapid sequence induction (RSI) (Cet 4-6ng.ml-1) in combination with an induction agent (ketamine, thiopentone or propofol) and suxamethonium or rocuronium.
Intubation without muscle relaxant
Remifentanil profoundly obtunds airway reflexes and under most circumstances allows tracheal intubation without the use of muscle relaxants in both adults and children. In our experience, this technique is most successful when using TIVA compared to a volatile/remifentanil combination. Although somewhat controversial, avoiding muscle relaxants may have benefits in certain situations: e.g.
- In those with abnormal sensitivity to muscle relaxants e.g. allergy, myasthenia gravis, malignant hyperthermia etc.
- Where assistance of nerve stimulators is desirable e.g. for monitoring facial nerve function during mastoid/parotid surgery or if planning a regional block immediately after induction
- Where avoidance of incomplete reversal or recurisation is desirable
- Less risk of awareness.
Here is our recipe for intubation using remifentanil:
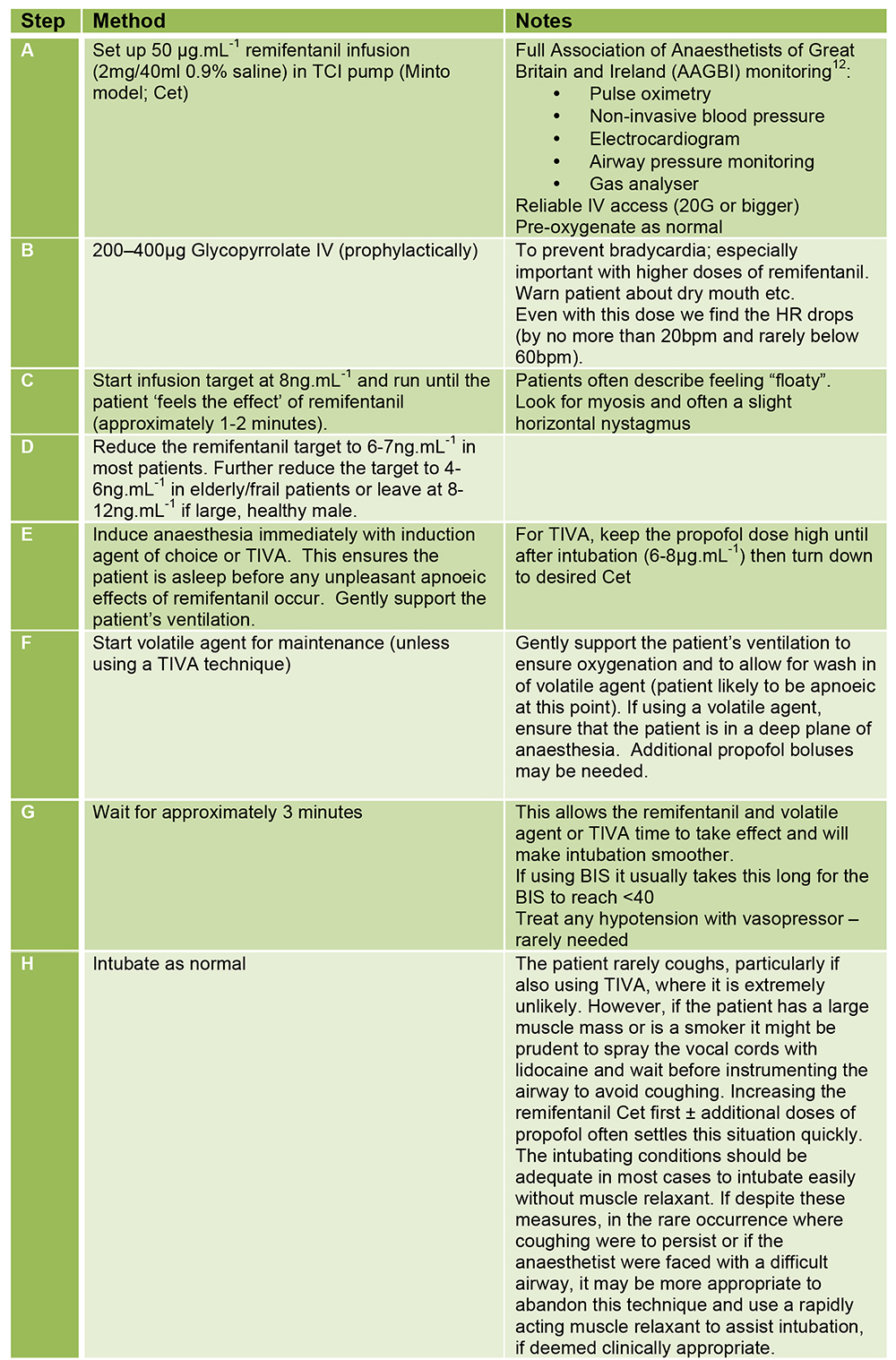
Figure 4. Suggested intubation protocol using remifentanil without muscle relaxant
Obstetrics
While epidural analgesia remains the gold standard for labour pain, remifentanil patient controlled analgesia (PCA) has now been cautiously accepted as an alternative in circumstances where epidurals are contraindicated (Figure 5). Remifentanil has been shown to receive equivalent or better satisfaction scores in comparison to epidural analgesia among laboring women13. Perhaps this is due to a perceived ease in administration and rapid effectiveness of remifentanil.
Remifentanil crosses the placental barrier however it is rapidly metabolized and redistributed by the foetus, even in the pre-term13. Remifentanil has a greater depressant effect on maternal respiratory function and consciousness than other opioids; this needs to be explained to parturients and must be vigilantly monitored in a 1:1 fashion by clinicians and midwives. Constant oxygen saturation monitoring is mandatory and supplemental oxygen and resuscitative equipment must be immediately available together with staff trained in their use14. There is no difference in maternal or neonatal morbidity or mortality when comparing epidural analgesia to remifentanil PCA; however, it is prudent to tell the neonatal team that remifentanil has been used during labour should the baby require any resuscitation13.
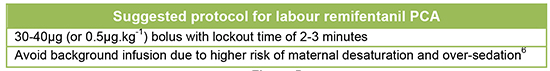
Figure 5
Remifentanil can also be useful during emergency Caesarian sections to avoid laryngoscopy-induced pressor response in eclamptic patients15. Aiming for Cet 4-6ng.ml-1 should be sufficient to achieve this as part of a RSI technique. Single intravenous boluses of remifentanil (0.6-1.3μg.kg-1) have also been described, but this warrants caution, as a bolus method delivers remifentanil much faster than TCI delivery and may lead to adverse cardiovascular effects, truncal rigidity and apnoea.
Awake fibre-optic Intubations (AFOI)
AFOI is a valuable technique for the difficult airway. Goals of AFOI include obtaining optimal intubating conditions and preserving spontaneous breathing whilst keeping the patient calm and comfortable and maintaining the options of revising and reversing the technique. Remifentanil is a useful accompaniment for AFOI, making the whole process smoother and more tolerable for patients.
Our recipe for AFOI with remifentanil is shown in Figure 6. Of note, only the sedation for AFOI is covered in this tutorial, the technique and complexities of AFOI can be found in ATOTW 201.
Conscious-sedation
Remifentanil can be used for many procedures where awake-sedation is required, examples include:
- Simple dental extractions
- Joint / fracture reductions in A+E
- Burns dressing changes
- Awake tracheostomy
- Bronchoscopy
- Adjunct-rescue to partially failed regional block or regional block that is wearing off
Safe use of remifentanil relies on appropriate patient selection. Remifentanil is not suitable for any patient that has a potentially difficult airway, is morbidly obese, is not starved, or for a potentially prolonged procedure. It also needs to be carried out in a location that is equipped to deal with any complications and have full AAGBI monitoring9 and resuscitation kit available. There are two schools of thought when it comes to providing supplemental oxygen during conscious-sedation – on the one hand providing a reservoir of oxygen in the lungs is useful in the event of any airway or breathing problems. On the other hand, an early fall in SpO2 helps to identify a patient who is over-sedated, allowing the remifentanil to be reduced or stopped more rapidly and the patient encouraged to breathe.
Our recipe for conscious-sedation is essentially the same as steps A-D of the AFOI recipe above (Figure 6), however we will reiterate that this must not be rushed – allow at least 2-3 minutes for the patient to respond to any dose increases. Avoid uncontrolled boluses as they can result in severe bradycardias and apnoeas, particularly in adults. Don’t forget prophylactic glycopyrrolate. Ensure that the patient’s IBW weight used in the Minto model is accurate.
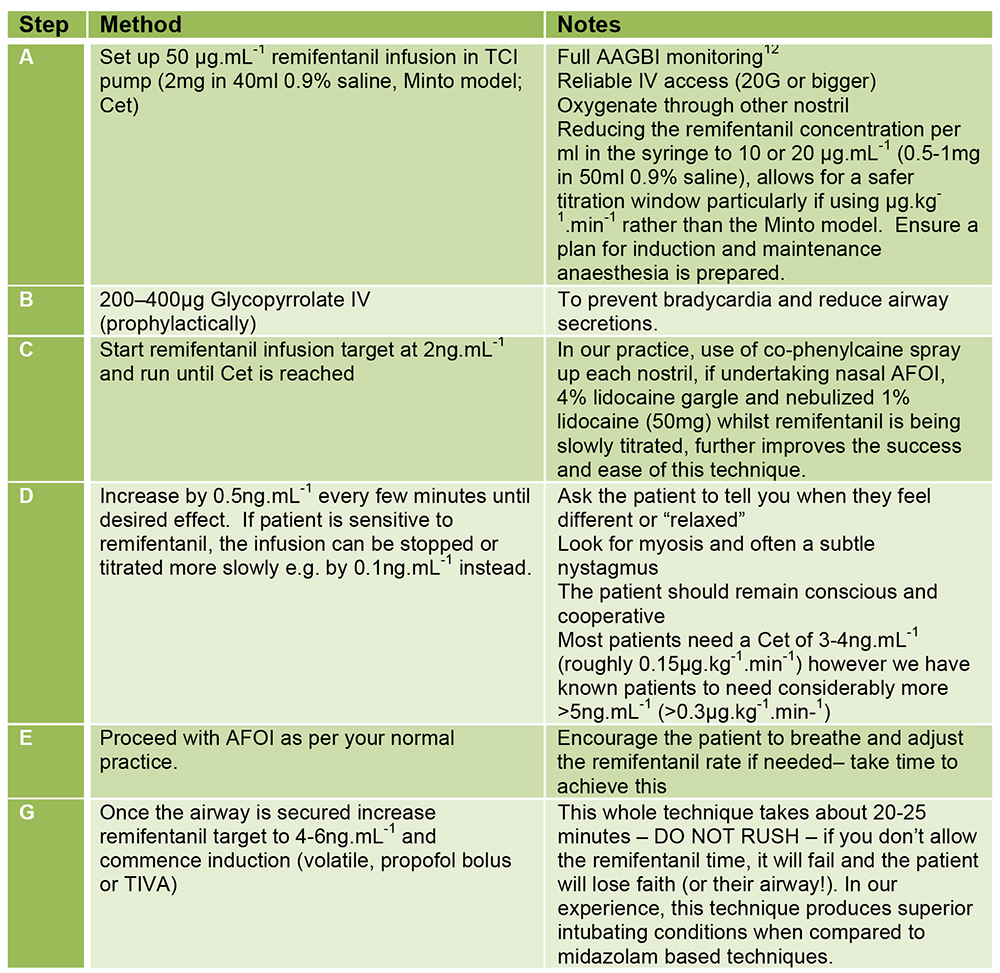
Figure 6. Suggested remifentanil protocol for awake fibre-optic intubation
Intensive care medicine
Optimal analgesia and sedation plays a crucial role in the management of patients on the ICU. Analgesia and sedation is commonly provided with propofol and an opioid (usually alfentanil in the UK). There is increasing evidence that daily sedation breaks and spontaneous breathing trials in mechanically ventilated patients are associated with shorter ICU stays and improved outcomes16,17,18. Remifentanil has a number of benefits over other short acting opioids. As a result, many intensive care units are now using it as a first line therapy. These benefits include:
- Rapid offset allowing for earlier neurological assessment during sedation holds.
- Profound respiratory depression helping to avoid patient-ventilator dysynchrony – less of an issue with modern ventilator modes.
- Very short context-sensitive half-life and minimal accumulation (unlike alfentanil or morphine) –ideal for resuming spontaneous breathing rapidly2.
- No need to dose-adjust in chronic or acute kidney injury (AKI) – offset times are approximately twice as long in moderate severe renal impairment however as the difference is only 16.5 mins this is not usually significant2.
- More predictable offset times particularly in patients with multi-organ dysfunction.
Since remifentanil is now more readily available the costs associated with its use have dropped significantly such that the cost of a 24-hour infusion of remifentanil is comparable to that of a 24-hour infusion of alfentanil. (UK prices; Remifentanil = £5.72 for 2mg, Alfentanil = £3.20 for 5mg19). In our practice, remifentanil is used first line with propofol for analgesia/sedation on the ICU.
Disadvantages to using remifentanil in the intensive care setting can be safely managed and should not discourage use. These disadvantages include:
- Potential for hyperalgesia and withdrawal following cessation of remifentanil infusion, warranting the use of post-remifentanil analgesia/opiate to be in place prior to dose reduction.
- Potential risk of apnoea and/or chest wall rigidity (in high doses) which may make ventilation more difficult. The apnoea risk needs to be taken seriously, particularly when using in patients who are not intubated. Staff need to remain vigilant of this potential complication when in use and have a plan in place if apnoeas were to occur.
- Cardiovascular instability (namely hypotension/bradycardia) may increase a patient’s vasopressor/inotrope requirement.
Remifentanil is less suitable for patients who do not have a secure airway, i.e. endotracheal tube. However, if patients are selected carefully and as experience grows, use in critical care patients without an endotracheal tube is likely to increase, for example, in aiding patient compliance with non-invasive ventilation, to provide optimal analgesia for brief dressing changes or turns and to provide better analgesia during invasive procedures.
Suggested infusion rates for a continuous infusion of remifentanil on the ICU would be 0.1 – 0.15μg.kg-1.min-1 (6 –9ng.mL-1) in ventilated patients to run alongside a propofol infusion. In non-ventilated patients, a remifentanil infusion of 0.05-0.1μg.kg-1.min-1 may be more appropriate depending on patient factors. Protocol guided use of a remifentanil in intensive care, may allow safe nurse-led dosing and weaning.
TIPS FOR SAFE USE OF REMIFENTANIL
- Avoid boluses – use the Minto model and change infusion rates instead.
- Pre-medication with an anticholinergic (200 – 400μg glycopyrollate) or with a sympathomimetic (3 – 6mg ephedrine) will help counteract any bradycardic side-effects.
- Ensure you have reliable IV access and infusion pumps and change syringes promptly – the rapid offset of remifentanil can be problematic if an infusion finishes unexpectedly.
- Remove/change IV sets and flush cannulas at the end of the operation to avoid inadvertent doses in recovery, or worse, back on the ward.
- Be patient and titrate slowly when using remifentanil for conscious sedation, including AFOI. Impatience is likely to cause more side effects.
SUMMARY
Remifentanil is an excellent, versatile drug with many possibilities for use within anaesthesia and critical care. Through education and appropriate use, remifentanil has the potential to significantly improve the conduct of cases and ultimately the quality of care experienced by our patients.
ANSWERS TO QUESTIONS
- Regarding the pharmacology of remifentanil:
a. True: LBW is more closely related to the pharmacodynamics than ABW
b. False: No dose adjustment is needed for renal failure
c. False: Post op shivering is twice as likely to occur with remifentanil
d. True: The half-life of remifentanil is approximately 3 minutes
e. False: Remifentanil is broken down by plasma and tissue non-specific esterases. Its effects are not prolonged in pseudocholinesterase deficiencies - Regarding target controlled infusions of remifentanil and total intravenous anaesthesia (TIVA):
a. False: The Minto model is used for remifentanil TCI whereas the Marsh model is used for propofol TCI
b. False: Age is also required for the Minto model
c. True: Remifentanil exhibits synergism with propofol allowing lower propofol concentration during TIVA
d. False: It should be kept between 2 – 8 nanograms per ml (ng. ml-1) not micrograms per ml (μg.ml-1)
e. False: The bolus dose delivered with effect-site targeting (Cet) is 3-4 times greater when compared to plasma-site targeting (Cpt) - Clinical applications of remifentanil include:
a. True
b. False: Please do NOT try this!
c. True
d. True
e. True: however vigilant monitoring of parturients using a remifentanil PCA is of the upmost importance to ensure patient safety
REFERENCES AND FURTHER READING
- Egan TD. Pharmacokinetics and pharmacodynamics of remifentanil: an update in the year 2000. Current Opinion in Anaesthesiology. 2000, 13:449-455.
- Breen D, Wilmer A, Bodenham A, Bach V, Bonde J, Kessler P, Albrecht S, Shaikh S. Offset of pharmacodynamic effects and safety of remifentanil in intensive care unit patients with various degrees of renal impairment. Critical Care. 2004, 8:R21-R30.
- Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC. Remifentanil for general anaesthesia: a systematic review. Anaesthesia 2007; 62: 1266-1280.
- Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a metaanalysis. British Journal of Anaesthesia 2014; 112(6): 991 – 1004.
- Mertens MJ, Engbers FHM, Burm AGL, Vuyk J. Predictive performance of computer-controlled infusion of remifentanil during propofol/remifentanil anaesthesia. British Journal or Anaesthesia 2003; 90(2): 132-141.
- Minto CF, Schnider TW, Egan TD et. al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. Model development. Anesthesiology. 1997; 86(1): 10-23.
- Mertens MJ, Olofsen E, Engbers FH, Burm AG, Bovill JG, Vuyk J. Propofol reduces perioperative remifentanil requirements in a synergistic manner: response surface modeling of perioperative remifentanil-propofol interactions. Anesthesiology. 2003; 99(2): 347-59.
- Tahari AK, Chien D, Azadi JR, et al. Optimum Lean Body Formulation for Correction of Standardised Uptake Value in PET Imaging. Journal of Nuclear Medicine. 2014; 55: 1-4
- Albertin A, Poli D, La Colla L, et al. Predictive performance of ‘Servin’s formula’ during BIS-guided propofolremifentanil target-controlled infusion in morbidly obese patients. British Journal of Anaesthesia. 2007; 98(1): 66-75
- Lemmens HJ, Brodsky JB, Bernstein DP. Estimating ideal body weight – a new formula. Obesity Surgery. 2005; 15(7): 1082-3
- Milne SE, Kenny GNC, Schraag S. Propofol sparing effect of remifentanil using closed-loop anaesthesia. British Journal of Anaesthesia. 2003; 90(5): 623-9
- Checketts MR, Alladi R, Furguson K et al. Recommendations for standards of monitoring during anaesthesia and recovery 2015: Association of Anaesthetists of Great Britain and Ireland. Published: December 2015.
- Freeman LM, Bloemenkamp KW, Franssen MT et al. Patient controlled analgesia with remifentanil versus epidural analgesia in labour: randomized multicenter equivalence trial. British Medical Journal. 2015;350:h846
- Douma MR, Verwey RA, Kam-Endtz CE, van der Linden PD, Stienstra R. Obstetric analgesia: a comparison of patient-controlled meperidine, remifentanil, and fentanyl in labour. British Journal of Anaesthesia. 2009; doi: 10.1093/bja/ aep359
- Yoo KY, Kang DH, Jeong H, Jeong CW, Choi YY, Lee J. A dose-response study of remifentanil for attenuation of the hypertensive response to laryngoscopy and tracheal intubation in severely preeclamptic women undergoing caesarean delivery under general anaesthesia. International journal of obstetric anaesthesia. 2013; 22: 10-18.
- Girard T, Kress J, Fuchs B, Thomason J, Schweickert W, Pun B et al, Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): A randomised controlled trial. Lancet. 2008; 371: 126-134.
- Reade MC, Finfer S. Sedation and delirium in the Intensive Care Unit. New England Journal of Medicine. 2014;370: 444-54.
- Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical Care Medicine. 2013; 41: 263-306.
- Paediatric Formulary Committee. BNF for Children September 2016. London: BMJ Group, Pharmaceutical Press, and RCPCH Publications; 2016



