Paediatric Anaesthesia
QUESTIONS
Before continuing with the tutorial, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Which of the following statements are true or false?
- All babies who require newborn resuscitation can be predicted before birth.
- Most babies do not require any intervention at birth.
- The normal foetal heart rate is <100bpm.
- The foetal heart rate normally reduces with each contraction, and returns to baseline around 30 seconds after the contraction has finished.
- Timely intervention in a complicated labour and basic neonatal life support with facemask ventilation will improve perinatal outcomes.
- Describe the steps required in intrauterine foetal resuscitation
- In the absence of meconium, what is the initial step in newborn resuscitation?
- Assess the Apgar score
- Assess the oxygen saturation
- Tracheal intubation
- Open the airway by extending the head
- Provide warmth, dry and stimulate and position to open the airway
- Which of the following statements are true or false?
- Intrapartum suctioning is essential if there is meconium
- Oxygen must always be used in newborn resuscitation
- It is wise to start chest compressions before ventilation
- Intravenous glucose should be given routinely
- Intravenous adrenaline is always required in newborn resuscitation
CASE HISTORY
A 27-year old mother presented to hospital in labour. This was her second pregnancy and she had been in labour at home for more than 24 hours. She had a history of febrile illness around the first trimester that responded to anti-malarial treatment. On arrival at the hospital, she was exhausted, but in good general condition, blood pressure of 100/70, pulse 90 beats/minute. Examination revealed that she was in established labour but that the foetal head was impacted in the birth canal. Auscultation of the foetal heart revealed a baseline heart rate of 130 beats/min and that the foetal heart rate slowed with each contraction, and only returned to baseline 30 seconds after each contraction had ended. The liquor was meconium stained. A diagnosis of obstructed labour with foetal distress was made.
The mother was placed on her left side and was given 100% oxygen to breathe by facemask. IV access was obtained and she received a litre of 0.9% saline. She was consented for emergency Caesarean section. A full blood count was taken and she was cross-matched for one unit of blood. She was taken to the operating room where an emergency caesarean section was performed under spinal anaesthesia.
The baby was delivered 20 minutes later, and initial assessment revealed a pale, floppy, meconiumstained baby. The baby was taken to the resuscitation table where the resuscitation team took over. The baby was intubated and the airway suctioned rapidly as the tracheal tube was withdrawn. The baby was rapidly dried, covered and gently stimulated, then placed in a neutral position to open the airway and ventilated with air by facemask using a self-inflating bag. Five initial rescue breaths were given, followed by ventilation at 30 breaths per minute. The chest was seen to move well. The heart rate was assessed using a stethoscope; it was initially 60 beats per minute, but in less than one minute increased to 130 beats per minute. After five minutes the baby became centrally pink although remained peripherally cyanosed, and was starting to cry and move around more vigorously. The baby was transferred to the neonatal unit for further management. He was monitored with a pulse oximeter and received oxygen by nasal prongs. He was given a full course of antibiotics.
BACKGROUND PHYSIOLOGY
How does a baby receive oxygen before birth?
Oxygen is vital for survival both before and after birth. Before birth, oxygen and other nutrients diffuse from maternal blood to foetal blood across the placenta. The foetal lungs are expanded but the air sacs are filled with fluid instead of air and the foetal lungs do not take any part in respiration. The foetal pulmonary vessels are greatly constricted and most of the blood is diverted away from the lungs.
What changes occur at birth?
With the start of labour, hormonal changes from the mother and baby cause the cells that secrete fluid within the baby’s lungs to switch from secretion to absorption, in preparation for the baby’s birth. After birth, the baby is stimulated to breathe due to the loss of placental blood supply as the cord is clamped and the physical discomfort of exposure to air at room temperature.
The first few breaths are crucial. Fluid is absorbed from the lungs and airways to establish a resting lung volume. A 3kg baby can clear 100ml of fluid from lungs and trachea in the first few minutes of life. The lung perfusion increases as the resistance in the blood vessels in the lungs is dramatically reduced, and the lungs take over respiratory gas exchange.
The vast majority of babies do not require assistance in taking these first few breathes but those that who not start breathing adequately will require urgent assistance as otherwise they will become rapidly hypoxic.
What can go wrong during this transition?
All babies need to be dried and gently stimulated at birth to initiate respiratory efforts. Some babies may require additional assistance at birth for a variety of reasons:
- The airway may be blocked by poor positioning, or a blood clot or mucous, so that the baby is unable to establish respiration.
- The baby may have been hypoxic in utero or may have become hypoxic after birth. The normal response of a newborn to hypoxia is to become apnoeic (primary apnoea). The baby does not breathe or cry sufficiently well to force fluid out of the alveoli and to establish a resting lung volume. These babies require immediate ventilation with facemask and self-inflating bag to aerate the lungs. If this is achieved rapidly and efficiently, the outlook for these babies is good.
The baby may have become severely hypoxic and acidotic in utero or after birth. Such a baby will appear pale and floppy with a slow heart rate and will only making gasping respiratory attempts or remain apnoeic (terminal apnoea). Such severe hypoxia leads to poor myocardial function and bradycardia with inadequate circulation of oxygenated blood to the brainstem respiratory centres. Unless these babies receive immediate active resuscitation their outlook is very poor.
Can you predict the babies who are likely to get into difficulty?
A number of factors are commonly associated with the need for assistance at birth (or more complex resuscitation). These include:
Maternal factors
- Very young or older mother (age <15 years, >35years)
- Small mother (maternal size <150cm, pre-pregnancy weight <47kg)
- Previous complicated deliveries or perinatal deaths
Factors during pregnancy
- Multiple pregnancy
- Maternal ill health – anaemia, jaundice, diabetes, syphilis, HIV, malaria, drug and alcohol abuse
- Post term (>42 weeks)
Factors during labour
- Foetal distress during labour
- Obstructed labour, prolonged second stage
- Meconium stained liquor
- Prolapsed cord
- Breech or other malpresentation
- Rupture membranes >24 hours
- Maternal fever during labour
- PV bleeding after 8th month
- Delivery by Caesarean section under general anaesthesia or where the mother has received recent opioid analgesia
- Premature delivery
HOW IS FOETAL DISTRESS DETECTED DURING LABOUR?
Foetal distress results from foetal hypoxia and is an indication for immediate delivery of the baby.
A baby who suffers foetal distress may open their bowels and pass meconium in utero; this will appear as meconium stained liquor after the membranes have ruptured. Reduced foetal movements in early labour should lead to the suspicion of foetal distress. During active labour, foetal distress is indicated by an abnormal foetal heart rate, monitored by auscultation with a Pinard stethoscope or Doppler probe.
It is important to assess the foetal heart rate regularly during active labour. The normal foetal heart rate is 110-150 beats/minute.
- Foetal tachycardia (>150 beats/minute) should raise suspicions of foetal distress.
- Early decelerations are due to vagal stimulation as the baby’s head is squeezed through the birth canal – the foetal heart rate returns to baseline before the end of the contraction. This indicates a risk of foetal distress and should be monitored carefully.
- Late decelerations occur when the foetal heart rate slows with each contraction but returns to baseline more than 30 seconds after the end of the contraction. This is a sign of severe foetal distress.
- Foetal bradycardia is defined as a foetal heart rate <100 beats/minute. Both late decelerations and foetal bradycardia imply serious foetal distress; if they are combined, there is a high risk of foetal death and the baby must be delivered urgently.
The gold standard to detect foetal distress is by taking a foetal scalp blood sample to assess foetal hypoxia and acidosis. This can only be done after the membranes have ruptured and carries a risk of infection for the baby. It is not usually available in resource-limited areas.
INTRAUTERINE FOETAL RESUSCITATION
Problems during labour may result in compromise of placental blood supply to the foetus. Reduction in oxygen delivery to the foetus will cause foetal hypoxia with secondary metabolic acidosis and lactic acidosis from anaerobic metabolism. If foetal distress is detected, preparations should be made for emergency delivery of the baby.
Intra-uterine resuscitation may correct the oxygen supply balance or it may improve the foetal condition sufficiently to allow obstetric assessment and if a Caesarean section is required, may allow time for a regional anaesthetic to be performed. The anaesthetist can play a vital role in the obstetric team in the optimization of uterine oxygen delivery. The techniques described below are easily achieved and can make a positive difference to foetal outcome.
1. Relief of aortocaval compression
The mother should be placed in full left lateral position to relieve aortocaval compression. The highest maternal cardiac output is achieved in the left lateral position. Relief of aortocaval compression is associated with improved foetal oxygen saturations and heart rate. When there is no improvement in foetal heart rate and cord compression is suspected, attempt an alternate positioning of the mother, such as right lateral position. If cord prolapse is suspected, ask the mother to kneel forwards with her elbows on her knees; this will take the pressure of the presenting part off the cord.
2. Oxygen
In order to maximize the placental oxygen transfer from mother to foetus, the mother should be given supplementary oxygen at high flow (15 litres/minute), via a Hudson mask with a reservoir bag.
3. Tocolysis
Reduced uteroplacental blood flow whether caused by uterine hyperstimulation or umbilical cord compression can be improved with tocolysis. The most common cause of uterine hyperstimulation is as a result of induction of labour with prostaglandins or augmentation of labour with oxytocin. Stopping an oxytocin infusion is an important first step and may be all that is required. For more severe cases, terbutaline 250 microgram subcutaneously may be given. Alternative drugs include sublingual GTN spray or inhaled salbutamol (2 puffs initially, repeat after one minute, maximum 3 doses).
4. Maternal circulatory support
Uterine blood flow falls linearly with a fall in maternal blood pressure. With the exception of preeclamptic women, fluid resuscitation of 1 litre crystalloid solution is recommended in the treatment of foetal distress. Maternal hypotension as a result of haemorrhage will require continued fluid resuscitation including blood products. If there is foetal bradycardia with maternal hypotension, a vasopressor should be given. The agent of choice is ephedrine given in 3mg to 6mg boluses. Ephedrine causes foetal tachycardia and will also improve foetal cardiac output.
NEWBORN RESUSCITATION
Every baby requires drying, warmth and gentle stimulation at birth. Approximately 10% of newborns require assistance to begin breathing at birth and 1% requires extensive resuscitative measures to survive, although these figures may be higher in areas where access to obstetric care is delayed and there is a high incidence of foetal distress. It will not be possible to predict every case that requires resuscitation at birth in advance, and babies are often delivered at short notice. It is important to prepare the essential equipment well in advance.
The first duty of the anaesthetist in theatre during a Caesarean section is the care of the mother, and the midwives or paediatrician will be required to resuscitate the baby. The knowledge and skills of the anaesthetist are useful in resuscitation of the newborn so it is helpful for the anaesthetist to practice newborn resuscitation drills with the midwives in advance. Anyone that delivers a baby should be capable of basic resuscitation measures.
Essential equipment for resuscitation of the newborn
Essential resuscitation equipment should be available and clean wherever babies are delivered.
- Firm flat padded resuscitation surface
- Source of warmth (overhead heater, warm dry towels, radiator, hot water bottle wrapped in towels). Where facilities are available, preterm infants <30 weeks should be placed put in a clear plastic bag with the face exposed and the head covered, in order to preserve body temperature.
- Good light source
- Clock or timer to record time of birth, assessment (APGAR scores) and response to resuscitation
- Suction machine, suction catheters (bulb syringes)
- Airway equipment: facemask 0 and 1, oropharyngeal airways size 000, 00 and 0, 500ml self inflating bag with reservoir, neonatal face masks, laryngoscope and blade with spare light bulb Miller (1,0), Macintosh blade (0,1), tracheal tubes (2.5,3 for pre-term and 3.5 or 4.0 for term), stylets. Size 1 laryngeal masks may be useful if intubation is difficult.
- Nasogastric tube
- Adhesive tape
- Oxygen with room air mix available
- Stethoscope (to assess heart rate and breath sounds)
- Intravenous cannulae, G-24, umbilical catheter.
- Drugs: Normal saline, adrenaline 1:10,000, 10% glucose, sodium bicarbonate. Naloxone should be available, although it is not a drug of resuscitation.
Resuscitation sequences
The UK Resuscitation Council Newborn Life Support group recommended sequence of interventions for all newborn babies: dry, warm, assess: airway, breathing, circulation, drugs. The newborn life support algorithm is illustrated in figure 1.
All babies must be dried and covered and gently stimulated. They should be assessed immediately. Four signs should be assessed: colour and tone, breathing and heart rate. The assessment should be ongoing and continuous. The skin colour should be assessed – is the baby pink, centrally cyanosed or white? The tone should be assessed – is the baby active with good tone, or floppy and poorly responsive. Look at the chest movement, depth and rate. The heart rate cab be assessed by palpating the umbilical cord (but this is not always reliable), or better by listening with a stethoscope over the precordium.
The newborn baby may fall into one of the following categories:Healthy newborn. Good tone, cries within a few seconds, good heart rate (120-150bpm), may be blue initially but turns pink within 90 seconds.
Newborn in need of assistance. Blue at birth, less good tone, may have a slow heart rate (<100bpm), may not have established breathing by 90-12- seconds
Ill newborn. Pale, floppy, not breathing, slow or very slow heart rate.
It is vital to approach the resuscitation interventions ‘ABCD’ in sequence and to complete each step before moving on. Approximately 30 seconds is allotted to complete each step, to re-evaluate, and decide whether to progress to the next step. Do not move on to the breathing if the airway is not clear. Do not move on to the circulation if the airway and breathing are not sorted. If it takes you 2-3 minutes to clear the airway and establish ventilation, then so be it. If there is no oxygen getting into the blood from the lungs, the heart and brain will remain hypoxic and there is no point in doing chest compressions.
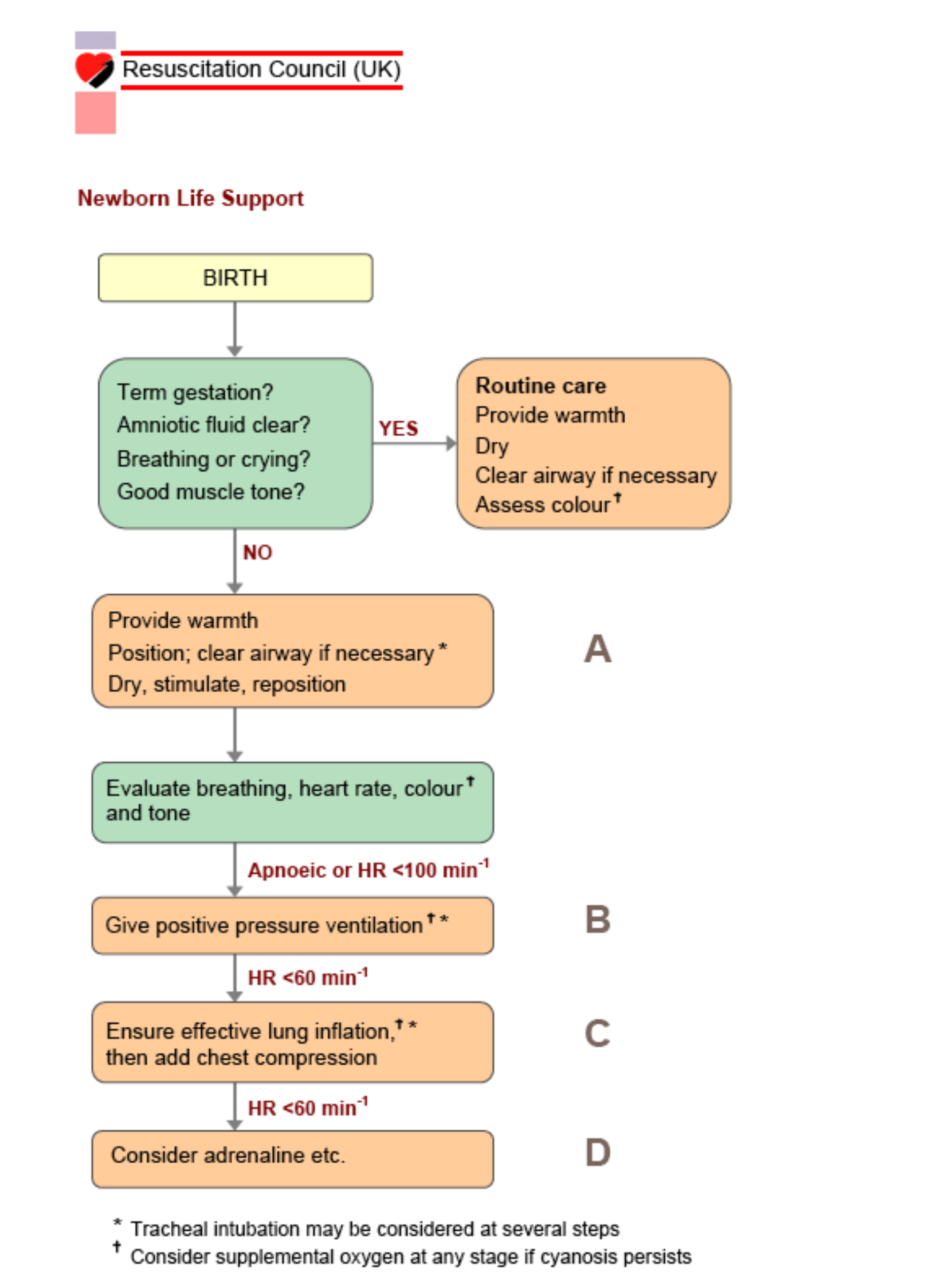
Figure 1. Newborn Life Support. Resuscitation Council (UK) 2005 (with permission)
AIRWAY
During initial steps in stabilization, position the baby supine on a flat surface, position the baby to open the airway – avoid neck flexion or overextension. Most babies should be able to clear their own airway with good positioning. The baby will only need suctioning if there is a foreign body like meconium or a blood clot. Blind or unnecessary suctioning should be avoided as this will result in vagal stimulation and bradycardia or breatholding.
BREATHING
Assess the breathing. If the baby remains gasping, apnoeic or bradycardic, or if there is persistent central cyanosis despite administration of supplementary oxygen, assist ventilation with rescue breaths with a self-inflating bag.
Initial Breaths and Assisted Ventilation:
First give five inflation breathes (2-3 sec duration, 30cm H20 inflation pressure). If the chest wall moves, move on to ventilation breathes (1-2 sec duration), aiming for 30 breaths/min until the child is vigorous. If chest wall does not move with your 1st five breathes:
- Recheck position
- Chin support
- Jaw thrust
- Double handed Jaw thrust
- Consider using a slighter longer inspiratory time or higher pressure
- Consider visualisation of the airway and suction to remove any obstruction.
The primary outcome of adequate initial ventilation is prompt improvement in the heart rate. Chest wall movement should be assessed if heart rate does not improve; the airway should be repositioned and ventilation reattempted.
Intubation
Tracheal intubation may be indicated at several points during neonatal resuscitation but should not be the primary intervention and should not be attempted by inexperienced operators. Ventilation using a facemask and self-inflating bag is the most important intervention in newborn resuscitation. Consider tracheal intubation:
- When tracheal suctioning for meconium is required (see below).
- If bag-mask ventilation is ineffective or prolonged ventilation is required
- When chest compressions are performed
- For special resuscitation circumstances, such as congenital diaphragmatic hernia or extremely low birth weight neonates (<1000 g)
CIRCULATION
Once the airway is clear and the chest is moving adequately, assess the heart rate. If the heart rate remains <60 beats per minute despite adequate ventilation, start chest compression.
The recommended technique of chest compression is with the hands encircling the chest with the fingers on the spine posteriorly, and the two thumbs pressing on the lower third of the sternum anteriorly to a depth of approximately one third of the anterior-posterior diameter of the chest.
Compressions and ventilations should be coordinated to avoid simultaneous delivery. The chest should be permitted to fully re-expand during relaxation, but the rescuer’s thumbs should not leave the chest.
There should be a 3:1 ratio of compressions to ventilations with 90 compressions and 30 breaths per minute. This will achieve approximately 120 events per minute and will maximize compressions and ventilation at an achievable rate.
DRUGS
Babies who have been significantly hypoxic and acidotic may require drugs to restore the circulation. However, drugs are not the first line intervention and will not be effective unless the airway is clear, the baby is adequately ventilated and chest compressions are underway.
The first line drug in newborn resuscitation is adrenaline, ideally delivered via an umbilical venous catheter, or alternatively via a peripheral cannula. The drugs used in newborn resuscitation are shown in table 1.
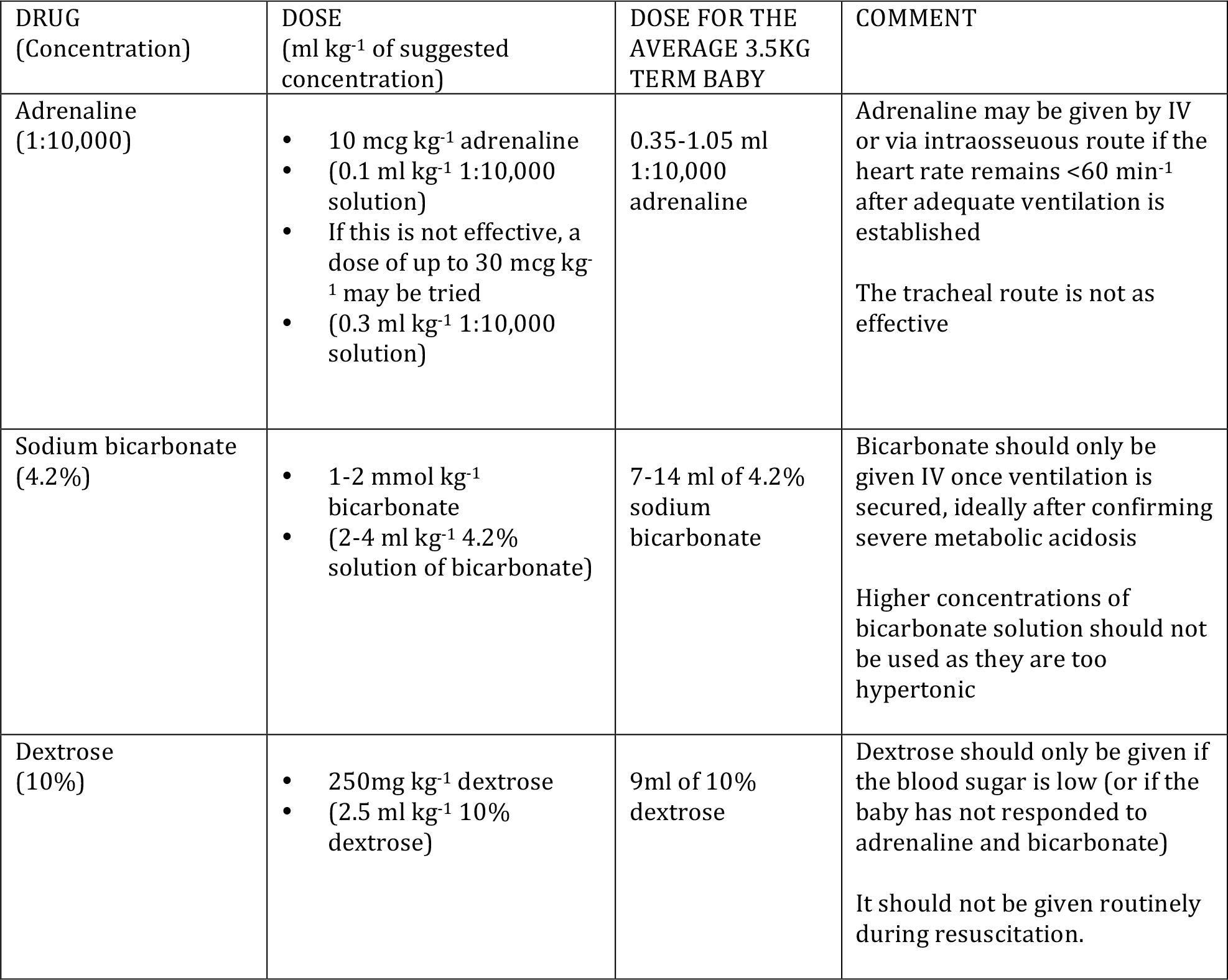
Table 1. Drugs used in resuscitation of the newborn
Clearing the airway of meconium
Inhalation of meconium before delivery or during birth can cause severe pneumonitis in the newborn. However, there is no evidence that routine suctioning of the airway when the head is on the perineum affects the incidence or severity of meconium aspiration syndrome, and intrapartum suctioning should no longer be practiced.
Intubation and direct tracheal suctioning of an infant who is vigorous at birth also offers no benefit, and may provoke vagal reflexes. Oral suctioning alone should be performed, without tracheal intubation. Do not suction the nose before the mouth, as this will stimulate the baby to gasp and to aspirate pharyngeal secretions.
If the baby is floppy at birth and is not making any respiratory efforts, and there is an individual skilled at tracheal intubation in the newborn, then the meconium stained baby should be intubated before drying and stimulation to clear the airway of possible meconium. If there is no equipment to clear the airway, proceed with the resuscitation sequence as normal.
Air versus oxygen
The use of oxygen in newborn resuscitation is controversial. There are concerns about high oxygen concentrations and damage induced by oxygen free radicals, particularly the effect on the lungs, brain and eyes. It has been shown that newborn infants may be resuscitated effectively either with air or oxygen. However, babies who have suffered a cardiac arrest will respond more rapidly if resuscitated with oxygen rather than air.
If air is used in the initial resuscitation but the baby fails to improve, or remains cyanosed, then supplementary oxygen should be added. If oxygen is used initially, then saturations should be monitored and maintained in the range 89%-94%. Prolonged high-inspired oxygen concentrations should be avoided and all oxygen therapy should be monitored with a pulse oximeter.
The Apgar score.
The traditional method of describing the condition of the newborn at birth is using the Apgar score (see table 2)
The score is assessed at 1 minute and repeated at 5-minute intervals to describe the response to resuscitation. Initial resuscitation measures should not be delayed to assess the Apgar score at one minute. A score of 3 is critically low; a score of 7-10 at 5 minutes is normal. Although the Apgar score is not intended to predict outcome or survival, a baby who scores less than 3 at 10, 15 and 20 minutes will have an extremely poor outcome without first class intensive care.
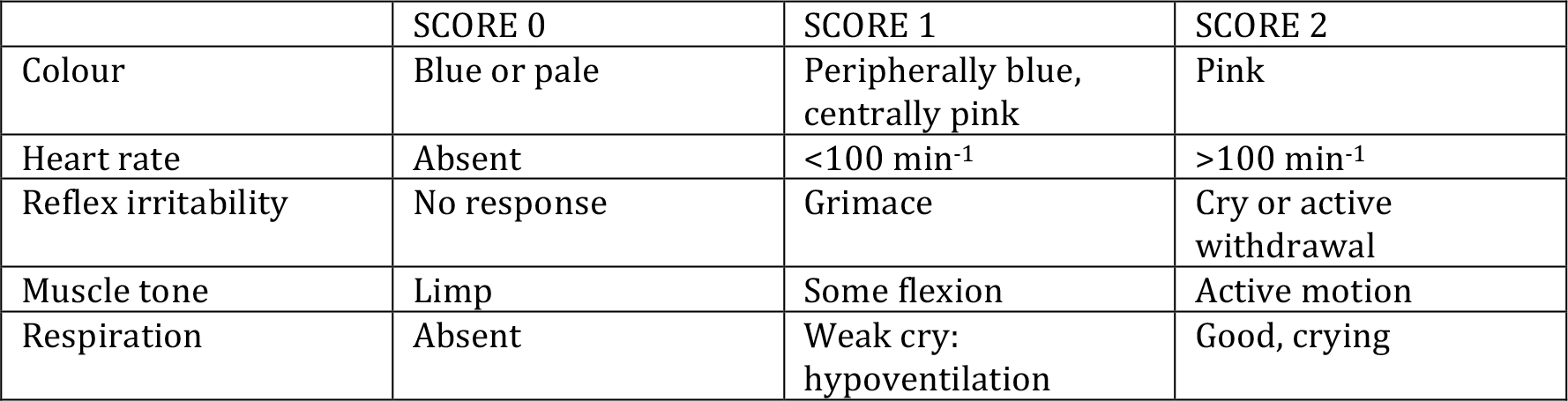
Table 2. The Apgar score. Assess at 1 minute and at 5-minute intervals as indicated.
Discontinuing Resuscitative Efforts
Infants without signs of life (no heart beat and no respiratory effort) after 10 minutes of resuscitation show either a high mortality or severe neurodevelopmental disability.
After 20 minutes of continuous and adequate resuscitative efforts, discontinuation of CPR can be justified.
Post resuscitation care
All babies who require active resuscitation should be transferred to an environment where close monitoring and anticipatory care can be provided. The baby should be kept warm, ideally in skin-to skin contact with the mother. Hyperthemia and hypothermia should be avoided. The baby should be encouraged to feed, ideally within an hour. Those who have received active resuscitation with one-two minutes support of bag bask ventilation should show rapid recovery.
Babies who have received full resuscitative measures including drugs require on-going support. Respiration be monitored, ideally using a pulse oximeter, particularly where there has been meconium aspiration. Oxygen should only be given if indicated, and saturations should be maintained in the range 89%-94%. Babies who develop signs of respiratory distress may require positive pressure airway support (cpap), or intubation and ventilation in a specialised neonatal unit.
Babies who have suffered significant hypoxic injury may have ischaemic damage to the brain, gut, kidneys or liver; these babies will also require specialised support.
ANSWERS TO QUESTIONS
1.
- All babies who require newborn resuscitation may be predicted before birth.False. Many babies who require resuscitation at birth can be predicted (see text), but not all. Preparations for basic newborn resuscitation must always be in place wherever a baby is born.
- Most babies do not require any intervention at birth. False. All babies need to be dried and kept warm.
- The normal foetal heart rate is <100bpm. False. The normal foetal heart rate is 110-150 bpm. A foetal heart rate of <100 is termed foetal bradycardia and indicates foetal distress
- The foetal heart rate normally reduces with each contraction, but returns to normal around 30 seconds after the contraction has finished. False. Late decelerations (especially with an underlying foetal bradycardia) indicates severe foetal distress, and a high risk of foetal death
- Timely intervention in a complicated labour will improve perinatal outcomes. True. There are around 2M perinatal deaths every year and around 1M survivors of birth asphyxia who develop cerebral palsy. Many cases of death and disability could be improved by timely intervention in complicated labour and basic newborn resuscitation.
2. Describe the steps required in intrauterine foetal resuscitation
Immediate steps:
- Place the mother in full left or right lateral position to avoid maternal supine hypotension. The mother should kneel forwards on her elbows if cord prolapse is suspected as this takes the pressure of the presenting part off the umbilical cord.
- Administer high flow oxygen to the mother using a well-fitting oxygen mask with reservoir bag.
Consider:
- 1000ml Ringers/Hartmann’s or Normal Saline IV to increase maternal blood pressure (caution in pre-eclampsia).
- Vasoconstrictor (e.g. ephedrine 6mg IV) if maternal hypotension is due to extensive sympathetic block from regional anaesthesia.
- Stop oxytocic agents to reduce uterine activity (if in use)
- Tocolytic agent (e.g. terbutaline 250 mcg SC or GTN sublingual spray, 2 puffs initially, repeat after 1 minute, maximum 3 doses).
3. In the absence of meconium, what is the initial step in newborn resuscitation?
Provide warmth, dry and stimulate and position to open the airway
4. Which of the following statements are true?
- Intrapartum suctioning is essential if there is meconium. False. There is no evidence that routine suctioning of the airway when the head is on the perineum affects the incidence or severity of meconium aspiration syndrome, and intrapartum suctioning should no longer be practiced.
- Oxygen must always be used in newborn resuscitation. False. Newborn babies may be equally well resuscitated with air or oxygen. However, a baby who has suffered a cardiac arrest may respond more rapidly if oxygen is used.
- It is wise to start chest compressions before ventilation. False. In newborn resuscitation, the lungs are filled with fluid and ventilation is the most important intervention.
- Intravenous glucose should be given routinely. False. Glucose should only be given where there is documented hypoglycaemia (or in the absence of measuring equipment, only when the baby does not respond to other medication). Hyperglycaemia may worsen neurological outcomes.
- Intravenous adrenaline is always required in newborn resuscitation. False. Drugs are rarely required in newborn resuscitation; effective ventilation is more important. If drugs are required, they predict poor outcome.
FURTHER READING
- Richmond S. Newborn Life Support. Resuscitation Council (UK) http://www.resus.org.uk/pages/nls.pdf (accessed 15th November 2005)
- Wall S, Lee AC , Niermeyer S et al. Neonatal resuscitation in low-resource settings: what, who and how to overcome challenges to scale up? International Journal of Obstetrics 2009 107:S47-S64
- Woods DL Newborn Care Manual. Perinatal Education Programme. International Association of Maternal and Neonatal Health. http://www.gfmer.ch/PEP/NCM_Home.htm (accessed 15th November 2009).



