Regional Anaesthesia
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Which of the following statements is correct?
- The brachial plexus emerges between the anterior and middle scalene muscles.
- The brachial plexus lies anterior to the subclavian artery as it passes over the first rib.
- Supraclavicular brachial plexus block carries a high risk of inadvertent injection of local anaesthetic into the subclavian vein.
- Block of the brachial plexus at the level of the first rib is ideal for shoulder surgery.
- Potential complications of supraclavicular brachial plexus block include:
- Mydriasis
- Pneumothorax
- Haemothorax
- Hoarseness
- The following nerves are likely NOT to be anaesthetised after supraclavicular brachial plexus block:
- Lateral cutaneous nerve of the fore-arm
- Phrenic nerve
- Intercostobrachial nerve
- Superficial cervical plexus
INTRODUCTION
The subclavian perivascular block is a supraclavicular approach to the brachial plexus. Unlike the traditional Kulenkampff technique, this is an interscalene block, but aiming to anaesthetise the 3 trunks of the brachial plexus as they cross the first rib rather than the nerve roots as they emerge between the scalene muscles. This is the point at which the brachial plexus is at its most compact. As a result it is possible to block the majority of the brachial plexus with one injection and with the lowest volume of local anaesthetic.
At the level of the first rib, the trunks are invested in a sheath (formed from the anterior part of the middle scalene muscle sheath and the posterior part of the anterior scalene sheath), which also includes the subclavian artery – hence the term subclavian perivascular.
ANATOMY
- The first rib runs approximately antero-posteriorly at the point where the trunks of the brachial plexus cross it.
- The plexus crosses the first rib between the insertions of the anterior scalene muscle (in front) and the middle scalene (behind)
- The brachial plexus lies posterior to the subclavian artery.
- The trunks are “stacked” – upper, middle and lower – but not necessarily in a straight vertical relationship.
- The lower trunk may lie under the subclavian artery.
- The subclavian vein is anterior to the anterior scalene muscle, and so should be well separated from the scene of action!
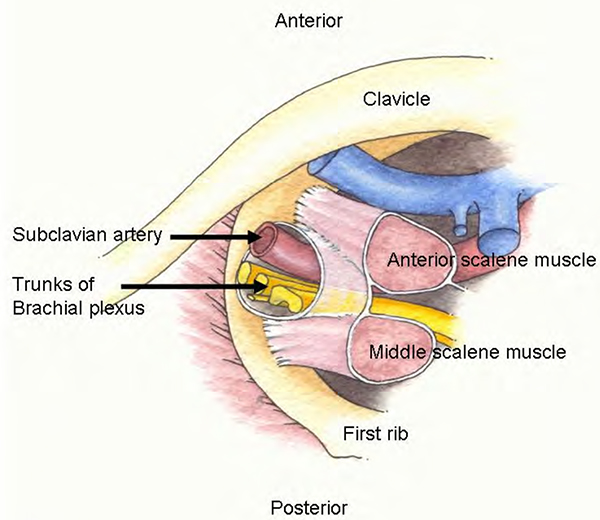
Figure1. Subclavian perivascular block anatomy: Brachial plexus viewed from above
WHAT IS BLOCKED?
- The trunks of the plexus, especially upper and middle.
- The sympathetic nerve supply to the upper limb.
- The lower trunk may be missed in 5% of blocks.
- The intercostobrachial nerve, which carries cutaneous sensation from the inner aspect of the upper arm, is missed in 90% of blocks – it does not normally originate from the brachial plexus.
INDICATIONS
- Good for humeral, elbow, fore-arm and hand surgery, especially areas supplied by the median and radial nerves, and the lateral and posterior cutaneous nerves of fore-arm.
- Possibly not the logical choice of brachial block for surgery confined to the medial side of the elbow, wrist and hand, or the little finger (because of the occasional failure to block the lower trunk of the plexus).
- Not for use in children under 12. The first rib is not fully calcified, and may therefore not stop the advancing needle penetrating pleura.
TECHNIQUE
- The plexus may be identified using either paraesthesiae or muscle stimulation.
- Using paraesthesiae, clear sensation must be elicited in any area below the shoulder / deltoid. Best results follow paraesthesiae in the hand or fingers. However, paraesthesiae limited to the thumb alone are associated with a poor block success rate.
- Using muscle stimulation, a twitch should preferably be elicited in muscles below the elbow i.e. flexors / extensors of wrist or fingers. Rotators of the forearm are less reliable. Ensure that any movement below the elbow is not simply “referred” from shoulder / upper arm muscle twitches.
- The highest success rate follows flexion of the fingers and thumb (Figure 2). Extension of the thumb alone is associated with poor block success.
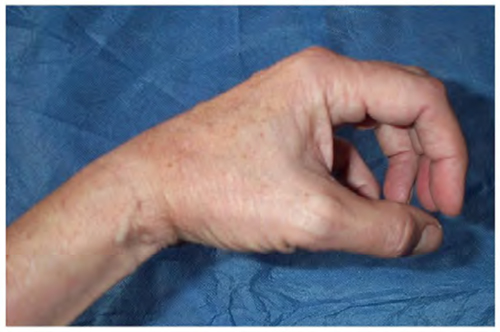
Figure 2. Finger and thumb flexion – the ideal response to nerve stimulation
- Use a 3.5 – 5 cm. 22G needle. Usually the plexus is found 1.5 – 3.0 cm. below the skin, but occasionally is deeper. I personally use short-bevelled needles.
- Using the nerve stimulator, start at 1 mA ONLY (2 Hz, 0.1 msec. pulse duration). The muscle twitches evoked using a higher current may be uncomfortable for the patient.
- Ideally a muscle twitch should still be apparent at a current of 0.3 – 0.5 mA. Withdraw slightly if a twitch is still present at 0.2 mA. I accept a current threshold of 0.8 mA if the quality of the twitch is good (i.e good finger flexion).
- The twitch or paraesthesiae do NOT need to be in the proposed surgical area.
- When using a stimulator, ignore paraesthesiae unless they remain with the stimulator switched off.
- With the patient lying flat, and the head turned only 30° to the opposite side, identify the interscalene groove (as for the Interscalene BPB). This is often a shallow dimple, not a deep chasm. Follow the groove down to the root of the neck. The subclavian artery is palpable in 50% of patients in this position.
- Insert the needle at the lowest point of the interscalene groove (where the skin is beginning to flatten out over the supraclavicular fossa), in the posterior part of the groove, and posterior to the subclavian artery if palpable (Figure 3).
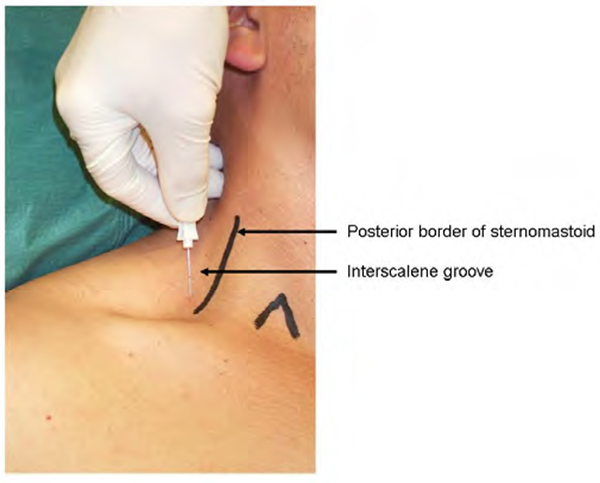
Figure 3. Needle insertion for Subclavian Perivascular block
- Direct the needle parallel to the floor and directly caudad – i.e. straight down towards the patient’s feet. THERE MUST BE ABSOLUTELY NO MEDIAL INTENT AS THE NEEDLE ADVANCES – otherwise the needle may penetrate pleura.
- If no paraesthesiae or twitch are elicited, withdraw the needle almost to skin and redirect fractionally more anteriorly or posteriorly. Only very small adjustments of angle should be made each time. It is easy to miss the plexus on either side if changes in angle are gross.
- If the subclavian artery is entered (I do on about 5% of occasions), withdraw the needle and redirect fractionally posteriorly. You will almost certainly encounter the plexus. I have on occasion entered the artery, directed the needle more posteriorly and not obtained any response. I have therefore deposited the local anaesthetic there anyway, and obtained an 80% rate of successful block.
- The Transarterial Technique is NOT successful in this approach to the brachial plexus.
- If the needle misses the brachial plexus, it is likely to insert on to the first rib. If so, walk antero-posteriorly along the rib.
DOSE
- This block needs about 0.5 ml/kg of LA solution, up to 30 mls. maximum.
- Many people use 0.5% bupivacaine for the total dose. This is well above the 2 mg/kg ceiling stipulated on the data sheet, but does not seem to cause problems. However anaesthesia may last 24 hours or more, which is worrying for the patient and the anaesthetist.
- I use a mixture of 0.5% bupivacaine and 1% lidocaine with adrenaline (or 1% prilocaine if available). This reduces the toxicity potential, and (in theory) allows a quicker onset. Analgesia lasts 12-18 hours with this mixture.
- Lidocaine 1.5% with adrenaline provides anaesthesia for 4 to 6 hours.
COMMON MISTAKES
- Selecting the groove between the sternomastoid and the anterior scalene. The anterior scalene muscle then separates the needle from the brachial plexus. The needle will be far too anterior. Many beginners cannot believe how posterior the insertion point is, and therefore use the very obvious sternomastoid-scalene groove.
- Advancing the needle with medial intent. Even very minor medial angulation of the needle risks slipping off the medial edge of the first rib into the pleura.
- Allowing too little time. It takes a minimum of 15 mins. to administer the block slickly (including time to insert an IV cannula and apply monitoring), and another 30 mins. for complete block after injecting LA.
SIDE EFFECTS
- Horner’s syndrome is common because of block of the sympathetic chain.
- Numbness and flail limb. As with all limb nerve blocks, the limb will be anaesthetic immediately afterwards; and muscle power will be lost. This is important if the patient is going home post-operatively, as the limb may be accidentally damaged (for instance, by fire) if it is not well protected in a sling.
- Phrenic nerve block and recurrent laryngeal nerve block. Phrenic nerve block is not as inevitable as with the Interscalene BPB, but may still occur in around 50% of patients. Recurrent laryngeal nerve block is rare with this block.
PROBLEMS
- The Intercostobrachial nerve is frequently not blocked, since it arises from the second thoracic nerve root, and therefore does not usually pass through the brachial plexus. Because it supplies cutaneous sensation to the inner aspect of the upper arm, it is important to block the nerve separately if a tourniquet is to be used. This may be carried out with a subcutaneous injection of 10 mls. of a short-acting local anaesthetic, e.g. lidocaine 1%, in the upper arm just distal to the axilla.
- Block failure. The ulnar nerve (lower trunk) is the most frequently missed, and may be related to the lower trunk lying under the artery.
- Pneumothorax. This is still possible, but is much less likely than with the Kulenkampff approach. In our institution, it has occurred three times in 24 years, during which time we have administered this block approximately 2,000 times. In all these patients, the degree of pneumothorax was small enough not to require a chest drain.
- Haematoma. If the subclavian artery is entered, it is difficult to apply pressure. This block is therefore not recommended in patients with a bleeding diathesis.
IMPORTANT POINTS
- The SPV is a good block for humeral, elbow, fore-arm and hand surgery
- Direct the needle parallel to the floor (with the patient lying flat) and directly caudad – no MEDIAL intent
- Pneumothorax is a potential complication
- An SPV block is not suitable for children younger than 12 years old
- An additional intercostobrachial block is likely to be needed to cover tourniquet pain in an awake patient
ANSWERS
-
- True.
- False. The brachial plexus lies posterior to the subclavian artery as it passes over the first rib.
- False. The subclavian vein is anterior to the anterior scalene muscle, and should therefore be some distance from the area of injection.
- False. An interscalene block at the level of the cricoid cartilage is more suitable for shoulder surgery because the higher nerve roots will be more securely anaesthetised, although block at the level of the first rib may anaesthetise the shoulder.
-
- False. A Horner’s syndrome may occur, which includes miosis.
- True.
- True. A haemothorax is a rare complication if a major blood vessel is punctured, especially in patients with a coagulopathy.
- True. Recurrent laryngeal nerve block is a rare side-effect, which wears off as the effect of the local anaesthetic recedes.
-
- False. Supraclavicular block is an excellent method of anaesthetising the musculo-cutaneous nerve, of which the lateral cutaneous nerve of the fore-arm is the terminal branch..
- False. The phrenic nerve may be anaesthetised in 50% of such blocks.
- True. The intercostobrachial nerve arises from the second intercostals nerve, and does not usually pass through the brachial plexus.
- True. The superficial cervical plexus is often included in the higher interscalene block.
REFERENCES and FURTHER READING
- Nicholls B, Conn D, Roberts A. The Abbott Pocket guide to Practical Peripheral Nerve Blockade.
ACKNOWLEDGEMENT
My thanks to Dr Alice Roberts, Department of Anatomy, University of Bristol for the use of her anatomy diagram for Figure 1.



