Basic Sciences
QUESTIONS
- The following are true or false:
- Airway patency can be lost without the use of muscle relaxants.
- Sevoflurane causes an increase in saliva production.
- Propofol causes a loss of the cough reflex.
- Saliva on the vocal cords can cause laryngospasm.
- Ketamine causes an increase in saliva production.
- End-tidal carbon dioxide:
- Corresponds to the arterial oxygen partial pressure.
- Is inversely proportional to the alveolar ventilation.
- Is raised after the administration of opioids.
- Is reduced if the cardiac output is significantly reduced.
- Can confirm the tracheal placement of an endotracheal tube.
- Ventilation:
- Is reduced by in the presence of an acidaemia.
- Is controlled only in the brain stem.
- Is stimulated by hypoxia.
- Is significantly impaired when using ether
- Is unaffected by the use of isoflurane.
- Hypoxia:
- Can always be corrected by increasing the inspired oxygen concentration.
- Can be caused by airway obstruction.
- Can not be prevented when inducing anaesthesia.
- Is caused by shunt when small airways collapse.
- Is made worse by hypoxic pulmonary vasoconstriction.
- The following are true or false:
- When the airway is obstructed, the main oxygen reserve is within arterial blood.
- The FRC is reduced by abdominal distension.
- Is greater than the closing capacity in an 80 year woman with COPD.
- Can be filled with oxygen by breathing 50% oxygen.
- A patient with a BMI of 35 breathing 100% oxygen will de-saturate faster than a patient with a BMI of 22.
INTRODUCTION
The primary functions of the respiratory system are:
- Ventilation; the movement of air into and out of the lungs.
- Gas exchange; the transfer of oxygen into the blood and the removal of carbon dioxide.
General anaesthesia has a number of effects on both of these key functions. The passage of gas into the lungs may be impaired by obstruction of the airway; the drive to ventilation may be reduced or cease altogether; the distribution of gas within the lungs may change and the transfer of oxygen (and anaesthetic gases) into the blood may be impaired. Most of these adverse effects can be seen during anaesthesia and in many patients these extend into the post-operative period. This tutorial will explain how anaesthesia affects the respiratory system and how these effects can be managed.
HOW ANAESTHESIA AFFECTS VENTILATION
1. Airway obstruction
General anaesthesia, with or without the use of neuromuscular blocking drugs, results in the loss of airway patency due to the relaxation of the pharyngeal muscles and posterior displacement of the tongue. The ability to manage secretions is lost, and saliva and mucous can obstruct the oropharynx. The loss of the cough reflex allows secretions (or refluxed gastric contents) onto the vocal cords, causing laryngospasm, or to enter the trachea and lungs causing bronchospasm and ultimately infection.
These effects result in airway obstruction and prevent the passage of gases into and out of the lungs resulting in hypoxia and hypercapnia.
2. Reduced ventilation
Carbon dioxide diffuses rapidly from the blood into the alveoli, from where it is removed by ventilation.
These events give rise to two key principles:
- The partial pressure of carbon dioxide in the alveoli (PACO2) is the same as the partial pressure of carbon dioxide in arterial blood (PaCO2).
- The PaCO2 is “ventilation dependent”; i.e. as alveolar ventilation increases more CO2 is excreted and the PaCO2 Conversely, a reduction in alveolar ventilation causes an increase in PaCO2.
The first principle allows us to use PACO2 as an indirect measure of PaCO2. This is done by sampling the expired gas and measuring the expired CO2. The gas at the end of expiration is the closest to pure alveolar gas. We call this the “end-tidal CO2” or PetCO2.
The second principle allows us to use PetCO2 as a measure of ventilation because the PetCO2 will change in the same direction as the PaCO2.
All anaesthetic drugs (except ketamine, ether and nitrous oxide) cause a dose- dependent reduction in ventilatory minute volume. This can be due to either a reduction in the respiratory rate (e.g. opioids), a reduction in the tidal volume (e.g. volatile anaesthetics) or both (e.g. propofol). As alveolar ventilation decreases the PaCO2 increases. Hypercapnia causes vasodilation, tachycardia, arrhythmias, hypertension and in an awake patient, headache, confusion, tremor, sedation and eventually coma (CO2 narcosis). Of equal importance is that the increased PACO2 displaces oxygen from the alveoli and can exacerbate hypoxia. All of these effects can be seen in the postoperative period.
Under normal conditions the PaCO2 of arterial blood is the predominant factor controlling ventilation. Any increase in PaCO2 is detected by peripheral (carotid bodies) and central (medullary) chemoreceptors. As a result there is a linear increase in ventilation of approximately 2 l/min for each 0.13 kPa (1 mmHg) rise in PaCO2. The pH (or hydrogen ion concentration) of the blood also has an effect. Acidaemia stimulates ventilation via the peripheral chemoreceptors. This ventilatory response to carbon dioxide is reduced by virtually all anaesthetic drugs (the main exception being ether) until excessively high concentrations are produced. As a result, anaesthetised patients become hypercapnic.
In addition, anaesthetics have two further undesirable effects on ventilation; firstly after a period of mechanical ventilation the threshold at which the PaCO2 stimulates the return of spontaneous ventilation is increased, thus delaying the return of spontaneous ventilation and secondly, the ventilatory response to acidosis is blunted, reducing a patient’s ability to compensate.
Hypoxia also effects ventilation. When the arterial oxygen concentration (PaO2) falls to less than 8 kPa (60 mmHg), the carotid and aortic body chemoreceptors increase minute ventilation and cardiac output through sympathetic nervous system stimulation. Anaesthetic drugs reduce this normal protective response to hypoxia, with volatile drugs having an effect at concentrations as low as 0.1 MAC (Minimum Alveolar Concentration). Clearly as patients recover from anaesthesia, low concentrations of a volatile drug last several hours into the post-operative period, putting them at risk of hypoxaemia.
HOW ANAESTHESIA EFFECTS GAS EXCHANGE
The second key function of the respiratory system is gas exchange. Oxygen is the gas of primary importance, but the exchange of anaesthetic gases will also be influenced.
Oxygenation is dependent upon:
- the inspired oxygen content
- the presence of a patent airway
- adequate alveolar ventilation
- appropriate matching between ventilation and perfusion in the lung
- the transfer of oxygen across the alveolar and endothelial membranes.
We have already looked at airway obstruction and hypoventilation, but anaesthesia also has other effects that reduce oxygenation.
1. Changes in functional residual capacity (FRC)
a. Oxygen content of FRC
FRC = ERV + RV
The volume of gas in the lungs at the end of normal expiration is the functional residual capacity (FRC), approximately 3000ml in a 70kg man.
ERV = Expiratory Reserve Volume, the volume that can be forcibly expired at the end of normal expiration
RV = Residual Volume, the volume left in the lungs at the end of maximal expiration
The oxygen in the FRC is the lung’s store of oxygen. Increasing the oxygen concentration of the inspired gas increases the proportion of oxygen in the FRC and hence increases the time taken for a patient to become hypoxic when ventilation stops. (Breathing air, 21% of 3000ml = 630ml oxygen. Breathing 30% oxygen, 30% of 3000ml = 900ml oxygen).
The oxygen in the FRC is the lung’s store of oxygen. Increasing the oxygen concentration of the inspired gas increases the proportion of oxygen in the FRC and hence increases the time taken for a patient to become hypoxic when ventilation stops. (Breathing air, 21% of 3000ml = 630ml oxygen. Breathing 30% oxygen, 30% of 3000ml = 900ml oxygen).
Preoxygenation (a high inspired oxygen content for several minutes/breaths before induction of anaesthesia) allows the FRC to act as a reservoir of oxygen and may prevent hypoxia for up to three minutes in a patient with normal lungs and oxygen consumption.
b. Volume of the FRC
The FRC is approximately 3000ml when upright but falls to around 2200ml in a supine position due to upward pressure from abdominal contents. General anaesthesia relaxes the diaphragm and intercostal muscles, with a further fall in FRC by 15-20% (approx 450ml). In addition, FRC is reduced by obesity, pregnancy, bowel distension or reduced alveolar volume due to atelectasis, consolidation or oedema. Therefore, an obese, supine patient may have reduced the volume of their FRC by 50%. This reduction in the store of oxygen will reduce the time taken to become hypoxic after ventilation ceases.
c. Relationship to closing capacity (CC)
CC = the lung volume at which small airways collapse, impeding flow of gas into the alveoli,
Usually FRC exceeds CC and prevents collapse during normal expiration. However, during anaesthesia the CC approaches the FRC producing small airway collapse in normal expiration with resultant atelectasis. This effect is also compounded in neonates, the elderly, smokers and patients with respiratory disease.
CT imaging of the thorax during anaesthesia, demonstrates this effect in up to 80% of patients.
2. Changes in ventilation and perfusion
In an ideal lung, the distribution of gas in the alveoli (ventilation, V) would be exactly matched by the distribution of blood flowing through the pulmonary capillaries (perfusion, Q). However, during inspiration, a greater proportion of the inhaled volume is distributed to the non-dependent areas at the top of the lung. Unfortunately, the effects of gravity reduce pulmonary blood flow in this region. As a result there is a degree of unevenness between ventilation and perfusion, usually referred to as “ventilation-to-perfusion (V/Q) mismatch”; the better-ventilated alveoli are under-perfused. This is often expressed as V/Q > 1. The oxygenation of blood in the pulmonary veins draining these regions is normal, but because of the relative excess ventilation, not all the available oxygen is absorbed. In extreme circumstances e.g. pulmonary embolus, perfusion is reduced to such an extent that insufficient blood perfuses the lungs and hypoxia does occur.
The opposite situation can and does exists, namely lack of ventilation of alveoli that are perfused with blood. In this case V/Q<1. This most often occurs as a result of alveolar collapse, preventing ventilation but not affecting perfusion; this is often referred to as “shunt”. As a result blood passing these alveoli does not become oxygenated, and remains as venous blood. This addition of deoxygenated venous blood to pulmonary vein blood causes a large reduction in arterial pO2. Hypoxaemia due to small shunts can be corrected by increasing the inspired O2 concentration, but once the amount of blood being shunted exceeds 30%, the hypoxia cannot be corrected even by breathing 100% oxygen.
Anaesthesia alters the distribution of gas and blood within the lungs. Both V/Q mismatch and shunt increase during anaesthesia, the latter (due to atelectasis) increases by around 5%. This has a profound effect reducing the oxygenation of the blood. Compensation for this effect by the blood flowing in areas of V/Q mismatch is limited as the blood from these areas is already almost fully saturated with oxygen. Consequently during most anaesthetics the inspired oxygen concentration is increased to offset the small degree of shunting. As outlined above,
3. Hypoxic pulmonary vasoconstriction (HPV)
HPV is the narrowing of pulmonary capillaries in areas of low alveolar oxygen content so that blood is diverted away from these areas helping to maintain arterial oxygenation. Volatile anaesthetic drugs suppress HPV, and blood flow to underventilated or collapsed alveoli is not reduced.
4. Other effects
Anaesthetic agents reduce respiratory tract ciliary activity, whilst dry gases result in mucus plugging. Some volatile drugs are directly irritant to the airways and produce coughing. Ketamine and neostigmine increase saliva and mucous production.
Anaesthesia causes a 15% reduction in metabolic rate with a reduction in oxygen requirement. Mechanical ventilation reduces oxygen requirements by a further 6%. However, the stress response to surgery, and post-operative shivering increase metabolic demand and may cause hypoxia.
HOW MECHANICAL VENTILLATION CAN DAMAGE LUNG TISSUE
Acute Respiratory Distress Syndrome ARDS
Mechanical ventilation can directly damage lung parenchyma. Large tidal volumes (>12ml/kg) cause alveoli shearing stress, releasing inflammatory mediators interleukin IL-6 and IL-8. These inflammatory mediators result in oedema in the interstitial wall of the alveoli, which reduces lung compliance and gas transfer causing hypoxia. This is termed the Acute Respiratory Distress Syndrome (ARDS) and results in prolonged stays on the intensive care unit (ICU) with a mortality of up to 40%.
Interleukin release, duration of ventilation and mortality may be reduced by “protective lung strategies” using high positive end-expiratory pressure (PEEP) to maintain alveolar patency and low tidal volumes (6ml/kg) to reduce shearing forces.
Pneumothorax (Barotrauma)
Pneumothorax occurs when air is trapped between the two pleural layers of the lungs with a loss of negative pressure that causes the lung to collapse. High inspiratory pressures or large tidal volumes can cause pneumothorax, which is more likely in the stiff, noncompliant lungs caused by ARDS or in the non-elastic lungs of chronic obstructive airways disease. The effect is exacerbated if there is an uneven distribution of disease (and therefore compliance) in the lung. The pressure required to keep one group of alveoli open may rupture another group causing a pneumothorax.
THE PHARMACOLOGICAL EFFECTS OF ANAESTHESIA
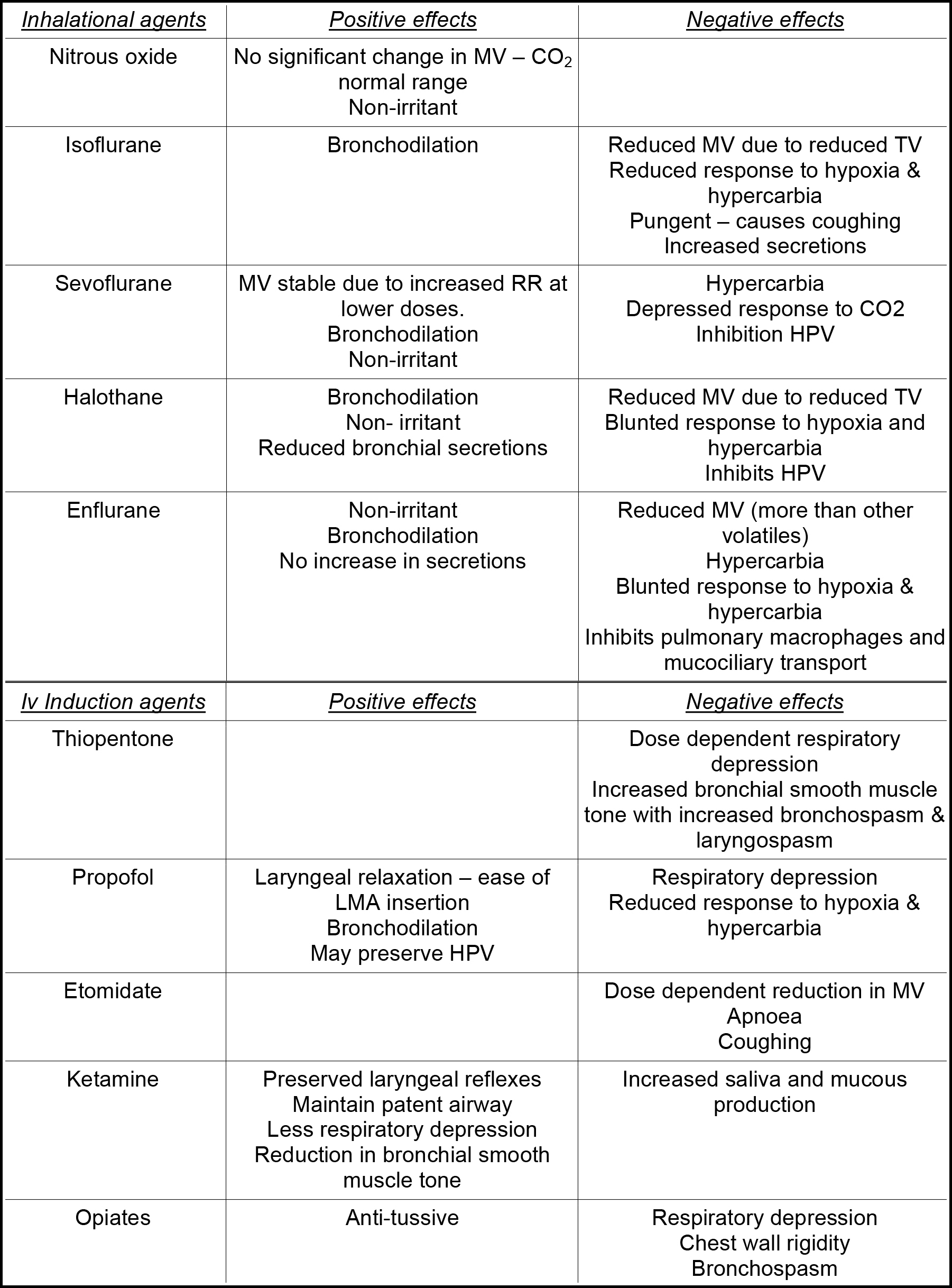
Table 1. Summary of the effects of the main anaesthetic drugs on the respiratory system.
- MV = Minute Ventilation
- TV = Tidal Volume
- RR = Respiratory Rate
- HPV = Hypoxic Pulmonary Vasoconstriction
- LMA = Laryngeal Mask Airway
MANAGING THE EFFECTS OF ANAESTHESIA ON THE RESPIRATORY SYSTEM
Preparation
- Positioning patients at a 45° angle prior to induction helps to reduce the fall in the FRC.
- Pre-oxygenation to maximize the oxygen content of the FRC can significantly increase the time from apnoea to hypoxia.
- Antimuscarinic drugs (atropine, glycopyrrolate) given before induction reduce the quantity of saliva in the airway.
Intra-operatively
The airway must be adequately maintained throughout the anaesthetic. Airway management is considered in other tutorials.
- Mechanical ventilation, in particular for obese patients, reduces airway collapse and atelectasis. Positive end-expiratory pressure (PEEP) helps to maintain alveolar patency and prevent hypoxia. If the patient is breathing spontaneously then continuous positive-airway pressure will have the same effect.
- PEEP and recruitment manoeuvres can be used to open collapsed portions of the lung. Recruitment is achieved by prolonged periods of high PEEP, for example, 5 breaths at 30cm H2O and then 10 breathes at 20cm H2 A PEEP of 5-10cm H2O throughout anaesthesia can maintain lung expansion, improving oxygenation and compliance, although recruitment may have to be repeated.
Lung protective strategies that are used to treat ARDS can also be used safely for obese patients, bariatric and laparoscopic surgery, and the elderly during anaesthesia to reduce atelectasis and increase oxygenation. This effect is not continued after extubation.
- Avoid long periods of 100% O2 which may produce “absorption atelectasis.” This is alveolar collapse following the complete absorption of 100% alveolar oxygen. The presence of the remaining nitrogen when breathing lower inspired concentrations of oxygen splints the alveoli open.
- Maintain adequate perfusion pressures with fluids and vasopressors to improve the perfusion of nondependent lung areas and reduce V/Q mismatch.
- Low (<1l/min) fresh gas flows in a circle circuit with a heat and moisture exchanger (HME) allow the rebreathing of expired gases causing heating and humification of inspired gas. This maintains mucous clearance and prevents tracheal dyskariosis and mucous plugging.
Post-operatively
Patients should receive oxygen immediately after an anaesthetic. This maintains an adequate alveolar oxygen concentration to correct the effects of hypoventilation, V/Q mismatch and the diffusion of anaesthetic gases into the alveoli. Oxygen can be continued into the post-operative period in patients at risk of hypoxia. Head-up tilt (as tolerated) increases the FRC and helps prevent atelectasis.
In obese patients in particular, extubation onto a CPAP mask may help to prevent airway collapse and atelectasis and maintain arterial oxygenation. Similarly, extubating ICU patients onto bi-level noninvasive ventilation has been shown to reduce the rate of re-intubation.
Make sure the patient has good postoperative analgesia. Patients should be able to take deep breaths and cough. Post-operative analgesia is discussed elsewhere.
SUMMARY
Understanding the multiple effects that general anaesthesia has on the respiratory system is essential if gas exchange and ventilation are to be maintained.
The loss of a patent airway, hypoventilation and apnoea cause hypercapnia, which has many undesirable effects. Anaesthetists must anticipate and prepare for these effects. A patent airway and ventilation must be maintained.
Gas exchange is impaired by airway obstruction, V/Q mismatch, shunt and the reversal of HPV, any of which results in hypoxia. The anaesthetist must strive to maximise the FRC and it’s oxygen content. Mechanical ventilation may be required which can be improved with recruitment, PEEP and lung protective strategies. However, remember that mechanical ventilation can cause damage to the lung tissue.
These problems extend into the postoperative period. Patients must have adequate postoperative analgesia, and some may require supplemental oxygen.
ANSWERS TO SELF-ASSESSMENT QUESTIONS
- T, F, T, T, T.
- F, T, T, T, T.
- F, F, T, F, F.
- F, T, F, T, F.
- F, T, F, F, T.



