General Topics
Objectives
By the end of this tutorial you will understand
- The factors that influence the risk of hospital acquired surgical site infections (SSI)
- Strategies to reduce the risk of hospital acquired surgical site infection
- The rational for antibiotic prophylaxis
- How to assess whether the use of antibiotic prophylaxis is indicated
Clinical scenario and self assessment questions:
Your patient is a 26 year old primagravida presenting for elective caesarean section. Your patient expresses concern about having an operative delivery because her friend recently developed a post –operative wound infection followed by a wound dehiscence in spite of receiving peri-operative antibiotics. The friend had a prolonged stay in hospital. Your patient has asked for further information about the risks of infection.
- What are the risk factors for surgical site infection (SSI)?
- What strategies are in place in your hospital to minimise the risk of surgical site infection.
- What are the benefits and risks of peri-operative antibiotic prophylaxis?
- Your patient is happy to proceed and the caesarean section is underway.
- When and how should antibiotic prophylaxis be administered for caesarean section?
- What organisms are likely to be the source of a bacteraemia occurring at the time of surgery?
- If your patient was not pregnant and was undergoing large bowel resection how and when should antibiotic prophylaxis be administered.
- The operation is complicated by considerable blood loss.
- How many doses of prophylactic antibiotics should be administered?
- The operation is completed and your patient has a healthy baby boy.
- A few days later you are in a budget meeting, the hospital is trying to cut costs and you are asked to consider:
- What factors determine the cost-effectiveness of prophylaxis and how are these factors used to guide recommendations for prophylaxis?
- Many years later this patient’s son is attending your hospital for tonsillectomy and adenoidectomy. He is now 8 years old. When you discuss his medical history with his mother she tells you that he is currently well and active however he developed rheumatic fever at the age of 6 years and was treated fully for that episode. She was told that he has a leaky valve; on examination your clinical findings suggest mitral regurgitation.
- Is he at risk of developing endocarditis during this procedure?
- How can you minimise the risk of him developing endocarditis?
- He developed a rash within 30 minutes of a previous exposure to penicillin and has not received penicillin since, how would you modify your prophylaxis strategy?
Infection is a leading cause of morbidity and mortality in hospitals in developing countries. Surgical site infections (SSIs) have become an important cause of morbidity in sub-saharan Africa. In countries where resources are limited even basic life saving operations such as appendicectomies and caesarean section are associated with high infection rates and mortality.
In developing countries with limited resources the focus of strategies for prevention of surgical site infection should be those procedures most frequently performed and those with the highest surgical infection site infection rate.
SSIs may be incisional, either superficial or deep; or can involve an organ or space that was opened or handled during an operation. On average having an SSI increases the patient’s hospital stay by 7-10 days.
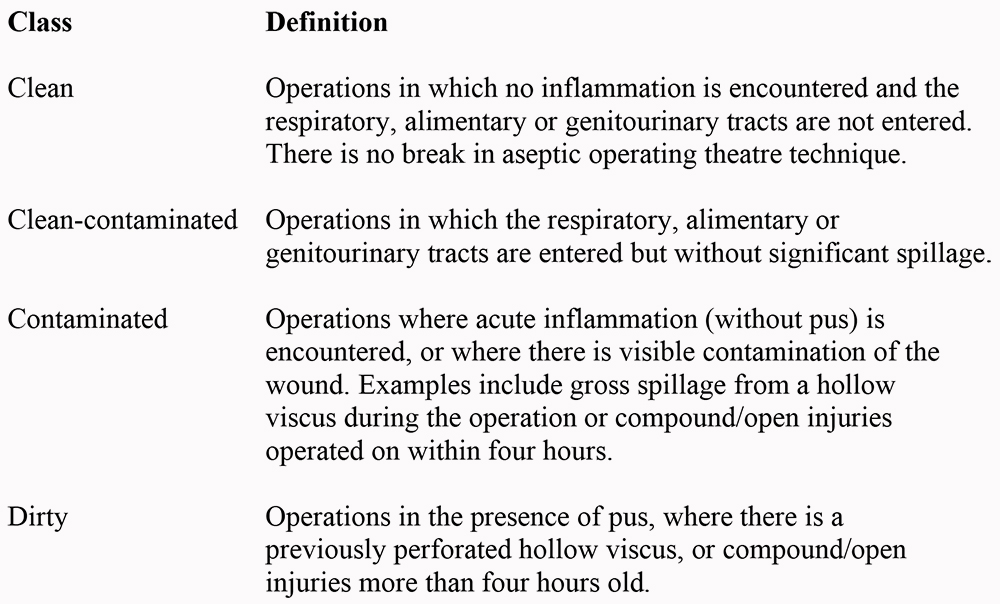
Operations can be categorised into four classes with an increasing incidence of bacterial contamination and subsequent incidence of post-operative infection.
CLASSIFICATION OF OPERATION
What is the source of the bacteraemia?
Organisms associated with SSIs vary with type of procedure and anatomic location of the operation.
- Coagulase negative staphylococcus (CNS), enterococcus species and E coli are 3 most frequently isolated pathogens.
- An increasing number of SSIs are caused by antimicrobial resistant pathogens and incidence of fungal SSIs has risen in part because of increasing numbers of patients with HIV/AIDS.
For most SSIs the source of the pathogen comes from the patient’s skin, mucous membranes or bowel and rarely from another infected site in the body i.e. endogenous sources. Exogenous sources of SSI pathogens are occasionally responsible e.g.
- Organisms from members of surgical team
- Contaminated surfaces in the operating room
- Contaminated instruments, surgical gloves or other items used in surgery.
- Exogenous organisms are primarily aerobic staphylococci or streptococci species.
What influences the development of infection?
By the end of an operation bacteria and micro-organisms contaminate all surgical wounds but only a small number of patients develop clinical infection. Factors influencing the development of infection include:
- Number of bacteria entering the wound
- Type and virulence i.e. the ability of those bacteria to cause infection
- Host immunocompetence
- External factors such as duration of surgery
Surgical skill and use of good technique can minimise the number of organisms entering the wound. The effectiveness of the inflammatory response depends on the patient’s general health and lifestyle.
Patient and operation characteristics that may influence the risk of developing a surgical site infection
Patient
- Co-morbidity
- Poor nutritional status
- Uncontrolled diabetes – diabetes should be controlled before elective surgery
- Obesity
- Coexisting infection at a remote body site
- Colonisation with micro-organisms
- Altered immunity e.g. HIV/AIDS, chronic use of corticosteroids
- Length of preoperative stay i.e. exposure to hospital acquired infection especially resistant organisms
- Smoking
Operation
- Preoperative shaving – see below
- Preoperative skin preparation – see below
- Duration of operation: it is estimated that infection rate nearly doubles with each hour of surgery
- Antimicrobial prophylaxis
- Operating room ventilation: positive pressure, air changes and air filtration are ideal but expensive to install and maintain
- Instrument processing
- Foreign material at the surgical site
- Surgical drains
- Surgical technique: specifically, it is important to:
- handle soft tissue gently to avoid crushing that can result in tissue death (necrosis);
- absorbable sutures whenever possible because permanent sutures, especially silk sutures, increase the likelihood of infection..
- use closed suction drains that exit through a separate stab wound to help prevent accumulation of tissue fluid in the dependent portion of the wound.
Hand Hygiene
Hand hygiene is a critical aspect of infection control. Improved hand washing practices result in decreased hospital acquired infection rates. Infections with antibiotic resistant bacteria such as MRSA (methicillin resistant staphylococcus aureus) are transmitted primarily by the contaminated hands of healthcare providers.
For routine hand hygiene plain soap and clean water are effective in reducing the risk of infection, provided the water quality is satisfactory. Soaps lower surface tension and mechanically remove dirt, debris and transient micro-organisms i.e. organisms which live in the upper layers of the skin. Transient micro-organisms are most likely to cause nosocomial infection they are acquired through contact with patients, other healthcare workers or contaminated surfaces during the course of the normal workday.
Resident micro-organisms live in the deeper layers of the skin and hair follicles and are more difficult to remove with soap and water however they are less likely to cause infection.
Antiseptics are chemicals which inhibit or kill micro-organisms e.g. alcohol, dilute iodine solutions and chlorhexidine.
Waterless alcohol-based antiseptic handrubs are fast acting and effective. They do not require water and remove transient flora and some resident micro-organisms. These usually contain 60-90% alcohol, an emollient (to protect the skin) and additional antiseptic e.g. chlorhexidine 2-4% which has residual action.
Gloves are not a substitute for hand hygiene but should be used in addition to hand hygiene. It is important to wash hands after removal of gloves because contamination of hands while removing gloves is common.
All members of the surgical team should perform full surgical hand scrub and use sterile gloves.
Skin Preparation Prior to Surgical Procedures
Although skin cannot be sterilised, applying an alcohol based antiseptic solution minimises the number of micro organisms around the surgical wound that may contaminate and cause infection. A wide area should be prepared around the proposed incision site.
Do not shave hair around the operative site. Shaving increases the risk of infection 5–10 fold because the tiny nicks in the skin provide an ideal setting for micro organisms to grow and multiply. If hair must be cut, trim the hair with a trimmer, close to the skin surface immediately before surgery.
Limit the number of people present during the operation during surgery and the traffic flow through the theatre. Keep the theatre doors closed.
Antibiotic prophylaxis in surgery
Antibiotic prophylaxis is never a substitute for asepsis and good surgical technique.
Antibiotics should be used in procedures with high infection rates and where consequences of infection are serious. The antibiotic chosen should be directed against the most likely infecting organism.
Any guidelines should be adapted with local microbiological expertise. Local antibiotic policy makers have the experience and information required to make recommendations about specific drug regimens based on an assessment of evidence and local information about microbiology and drug costs. Any planned antibiotic prophylaxis should take into consideration the clinical condition of the patient and the diagnostic and treatment options available. Hospital acquired infection with pseudomonas, staphylococcus (including MRSA) and multiresistant acinetobacters are increasingly a problem worldwide. Anti-microbial drug resistance is widespread and this can limit the number of effective anti-microbial agents. Always take local advice from your microbiologist about antibiotic resistance and which antibiotics to use in order to be both effective and to minimise the development of resistant strains.
Benefits must be weighed against risks of toxic and allergic reactions, emergence of resistance, superinfections and cost. A past history of a serious adverse reaction to an antibiotic is a contra-indication to its use.
Usually a single intravenous dose of an antibiotic given pre-operatively within 30 minutes of induction of anaesthesia provides adequate tissue levels throughout the operation. Post operative doses of antibiotic for prophylaxis should not be given. Consider repeat intraoperative doses if there is major blood loss or prolonged surgery. Antibiotic prophylaxis in caesarean section is delayed until clamping of the cord in order to prevent the drug reaching the neonate.
The dose of prophylactic antibiotic is usually the same as the therapeutic dose.
Prophylactic antibiotics should be administered at least 10 minutes before the application of a tourniquet to achieve appropriate tissue concentrations.
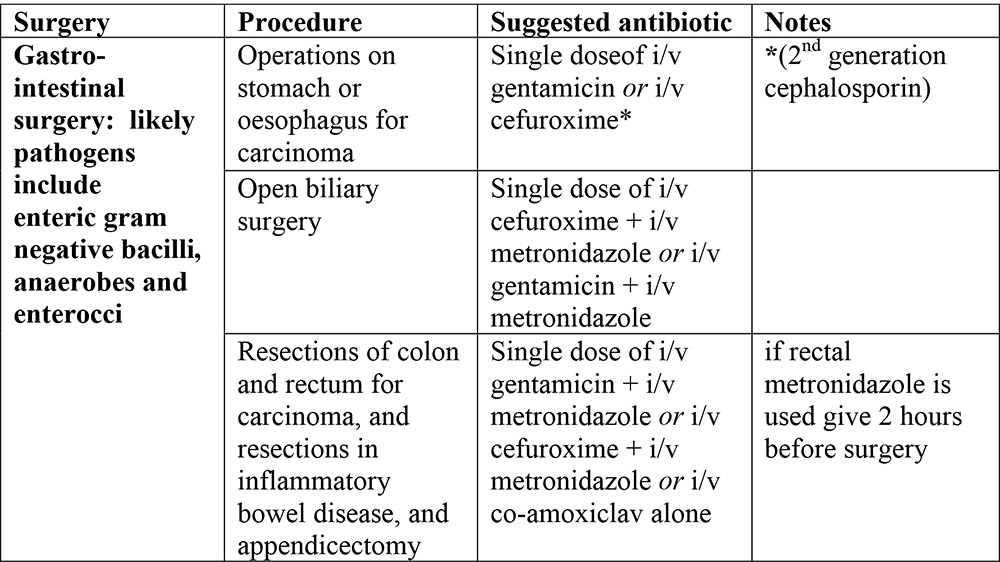
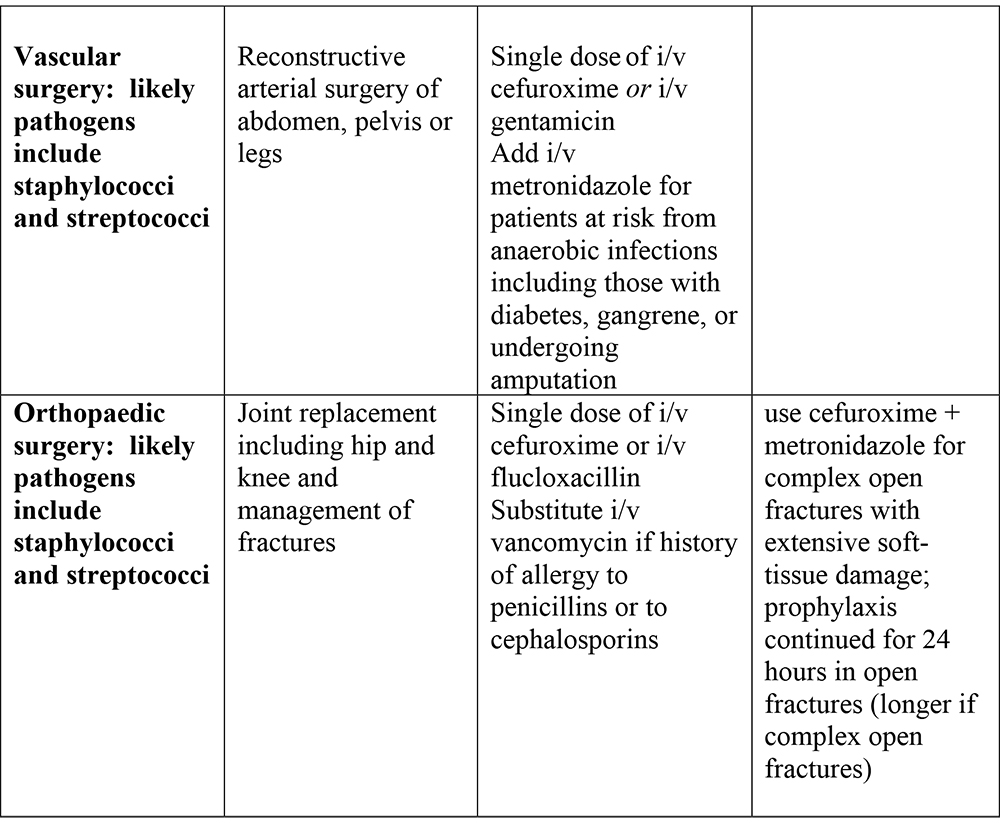
Suggested antibiotic prophylaxis for surgical procedures: these guidelines should be modified in accordance with local sensitivity data

Prevention of endocarditis
This is a controversial area, there are many guidelines. The evidence base is unclear as there is a lack of data in this area. Most recommendations are based on observational data. Some individuals who receive prophylaxis may still develop endocarditis.
Prevention does not solely concern antibiotic prophylaxis. For example, adequate treatment of infection that could cause bacteraemia or fungaemia, the prompt removal of colonised intravascular devices and effective management of conditions that can lead to chronic or repeated infections are essential in reducing the risk of subsequent endocarditis.
Endocarditis prophylaxis for non dental procedures
Enterococci, streptococci and staphylococci are the prominent causes of endocarditis associated with non-dental procedures in most settings. It is likely that the pathogenesis of endocarditis differs between the oral streptococci and other pathogens such as enterococci. The risk of endocarditis associated with various surgical procedures has been derived from an estimate of
- the chance of a procedure causing a bacteraemia and thus seeding an ‘at risk’ cardiac lesion and
- whether such a procedure has been anecdotally linked to cases of endocarditis.
However a risk of bacteraemia does not necessarily equate to a risk of endocarditis and the significance of both magnitude and duration of bacteraemia is unknown. Recommendations are a pragmatic compromise.
Procedures associated with bacteraemia and endocarditis and hence prophylaxis is recommended
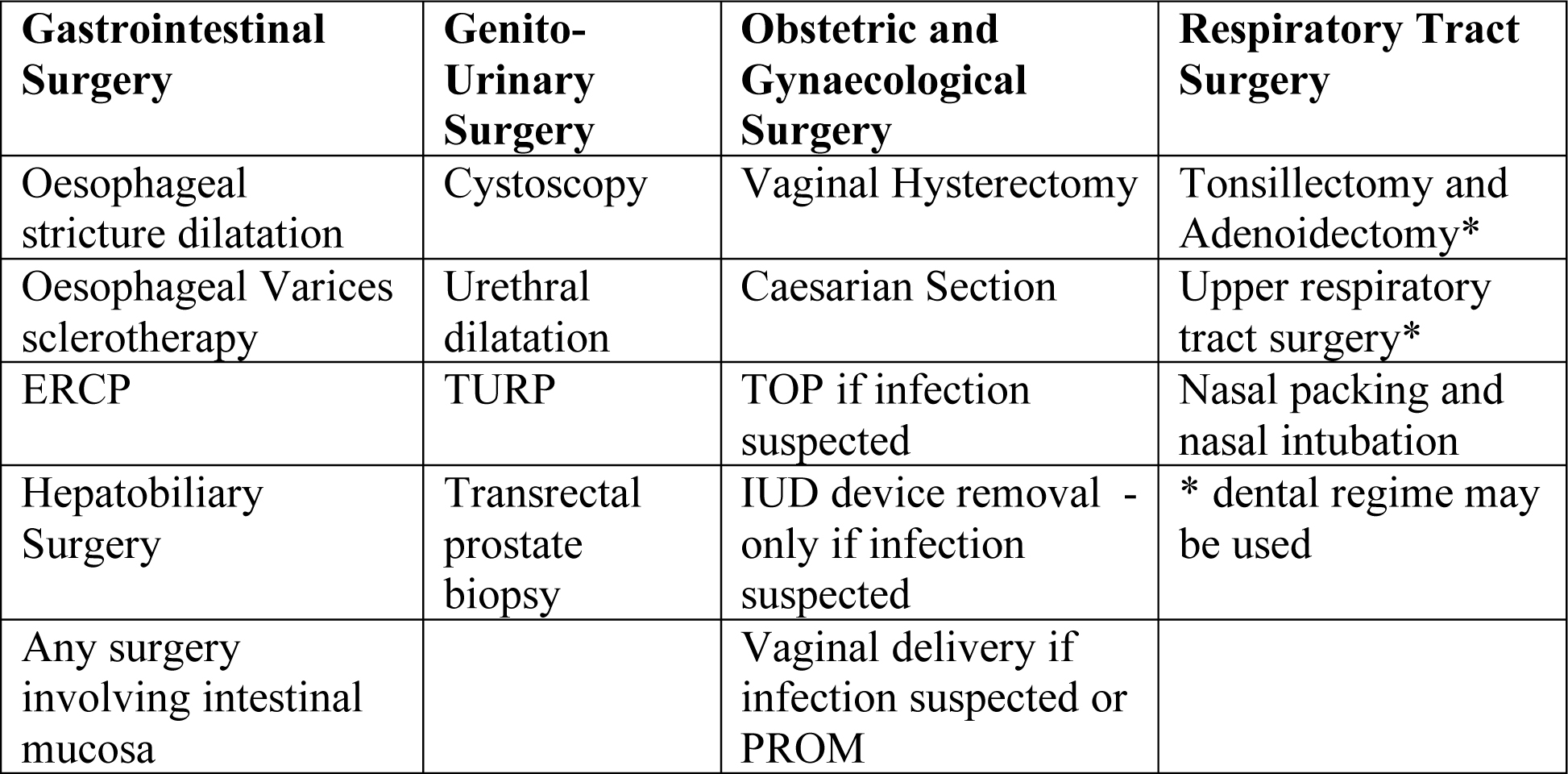
High risk patients e.g. those with previous infective endocarditis, those with mechanical or biological prosthetic valves or surgically constructed systemic or pulmonary shunts or conduits may need prophylaxis e.g. prior to upper/lower GI endoscopy.
Procedures involving a non infected skin incision and no mucosal breach do not require prophylaxis but of course skin disinfection prior to the procedure is mandatory.
Recommended prophylactic antibiotic regimens for genito-urinary, gastrointestinal, respiratory or obstetric and gynaecological procedures in patients at risk of endocarditis from Working Party of the British Society for Antimicrobial Chemotherapy 2006
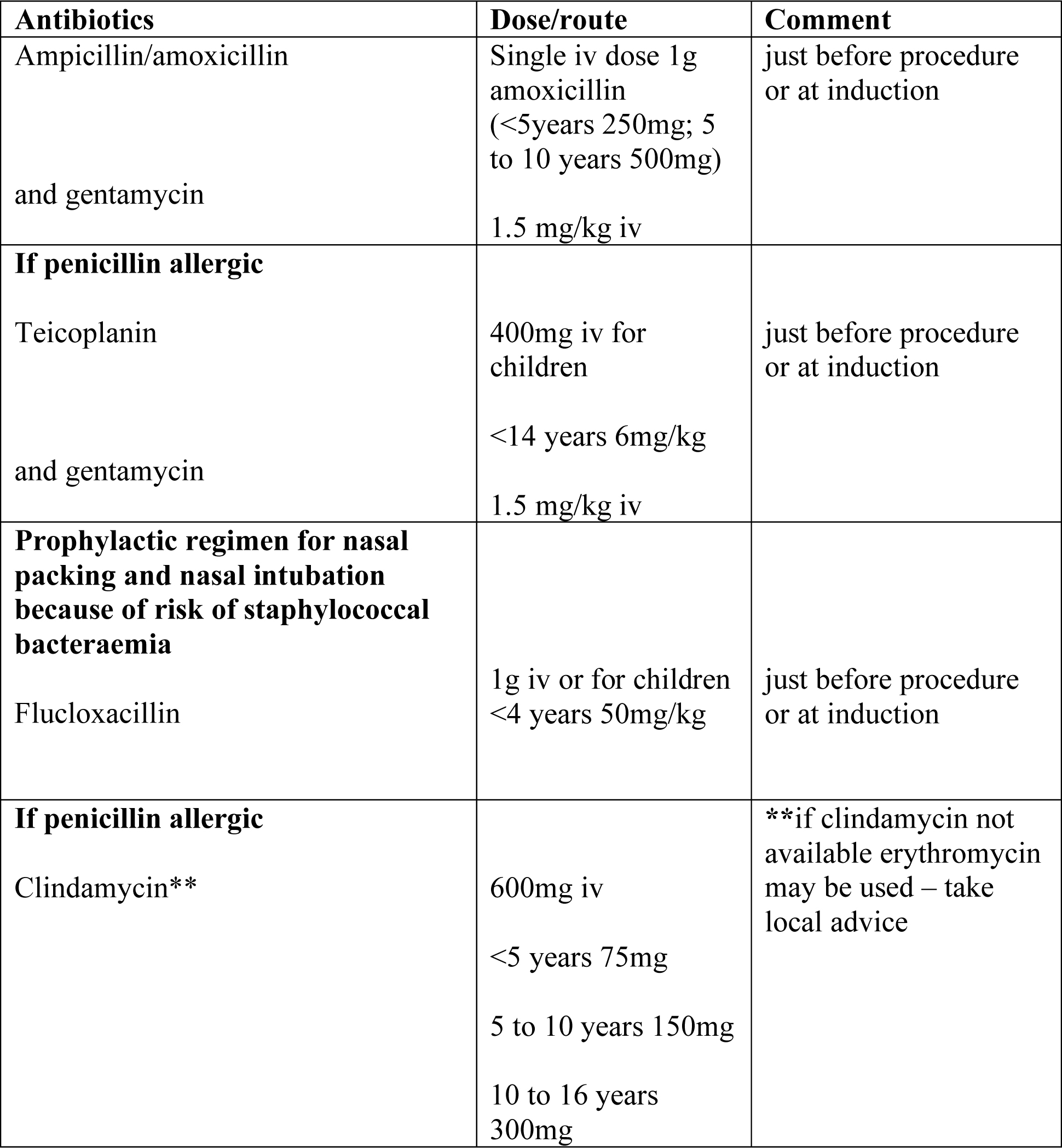
Jack is penicillin allergic so for his tonsillectomy the dental regime i.e. clindamycin or a combination of teicoplanin and gentamycin are appropriate.
Antibiotic prophylaxis for dental procedures from Working Party of the British Society for Antimicrobial Chemotherapy 2006
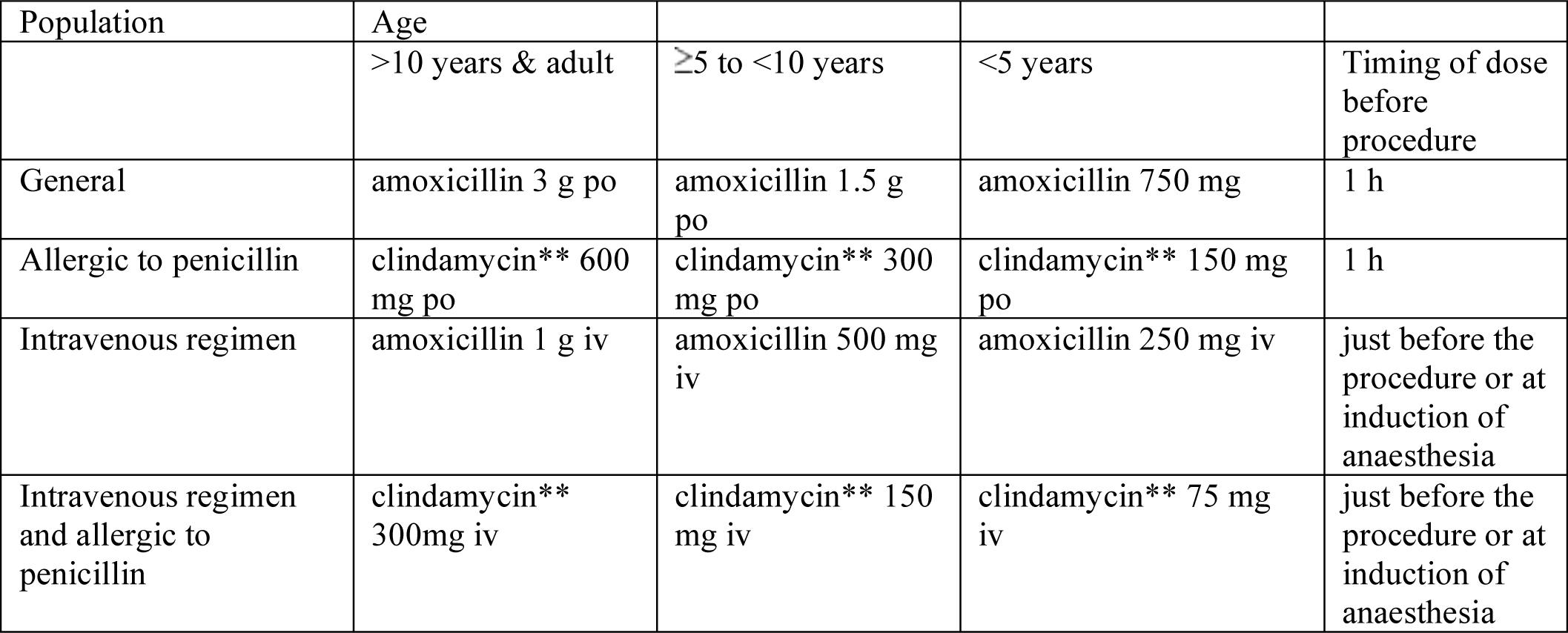
**if clindamycin not available erythromycin may be used – take local advice
Cardiac conditions for which antibiotic prophylaxis is indicated for non-dental procedures
- History of previous endocarditis
- Prosthetic cardiac valves
- Surgically constructed shunt/conduit
- Complex congenital heart disease (except secundum atrial septal defects)
- Complex LV outflow abnormalities, including aortic stenosis and bicuspid aortic valves.
- Acquired valvulopathy*
- Mitral valve prolapse*
* if echocardiography available with echocardiographic documentation of substantial leaflet pathology and regurgitation or valvulopathy suspected on clinical examination.
References:
- Infection Prevention Guidelines for Healthcare Facilities with Limited Resources. Linda Tietjen, Débora Bossemeyer, Noel McIntosh United
- States Agency for International Development
- http://www.reproline.jhu.edu follow links for infection prevention
- Prevention of hospital acquired infections
- World Health OrganizationDepartment of Communicable Disease,Surveillance and Response
- This document can be downloaded from the WHO/CSR Web site.
- http://www.who.int/emc follow links for publications WHO/CDS/CSR/EPH/2002/12
- Scottish Intercollegiate Guidelines Network: Antibiotic Prophylaxis in Surgery, July 2000
- http://www.sign.ac.uk follow links for guidelines by
- Gould FK, Elliott TSJ, Foweraker J, et al. (2006) Guidelines for the prevention of endocarditis: report of the Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 57:1035–42
- http://jac.oxfordjournals.org/cgi/content/abstract/dkl121v1 free full text
With thanks to: Prof Rumina Hasan (Chairperson Dept of Pathology/Microbiology, Aga Khan University, Pakistan), Dr Kamal Kishore (Associate Professor Medical Microbiology Fiji School of Medicine, Fiji) and Dr Isabeau Walker (Consultant Anaesthetist, Great Ormond Street Hospital for Children NHS Trust, London, UK)