QUESTIONS
Before reading the article, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- How many nerves supply the wrist joint?
- Three
- Four
- Five
- Six
- Which of the following statements is true?
- The ulnar nerve supplies the skin of the thumb.
- The recurrent branch of the median nerve supplies the three hypothenar muscles.
- The radial nerve arises from the lateral cord of the brachial plexus.
- The anterior interosseous nerve is a branch of the median nerve
- Which of the following statements is false?
- The posterior interosseous nerve is predominantly motor.
- Some of the sensory supply to the skin on the back of the hand comes from the ulnar nerve.
- The median nerve has several branches in the upper arm.
- The ulnar nerve supplies flexor carpi ulnaris and half of flexor digitorum profundus.
INTRODUCTION
A wrist block is the technique of blocking terminal branches of some or all of the six nerves that supply the wrist, hand and fingers. The combination of nerves that need to be blocked depends upon the exact location of surgery. This block can be used to provide regional anaesthesia for a patient undergoing surgery awake or as an analgesic technique to be used in combination with general anaesthesia or brachial plexus block (BPB) using short-acting local anaesthetic (the wrist block will provide prolonged pain relief once the BPB has worn off). It is simple to perform with readily identifiable landmarks, yet remains an under-used weapon in the anaesthetist’s armamentarium.
INTRODUCTION
A wrist block is the technique of blocking terminal branches of some or all of the six nerves that supply the wrist, hand and fingers. The combination of nerves that need to be blocked depends upon the exact location of surgery. This block can be used to provide regional anaesthesia for a patient undergoing surgery awake or as an analgesic technique to be used in combination with general anaesthesia or brachial plexus block (BPB) using short-acting local anaesthetic (the wrist block will provide prolonged pain relief once the BPB has worn off). It is simple to perform with readily identifiable landmarks, yet remains an under-used weapon in the anaesthetist’s armamentarium.
INDICATIONS
Anaesthesia and/or analgesia for many surgical procedures on the wrist, hand and fingers such as wrist arthroscopy, the correction of dupuytren’s contractures, metacarpal or phalangeal osteotomy, arthrodesis of the MCP joints, fixation of fractures in the hand. It is worth noting, however, that in an awake patient, the duration of surgery may be limited by the patient’s ability to tolerate the tourniquet on the upper arm if a wrist block alone is used.
CONTRA-INDICATIONS
Absolute Contra-indications
- Patient refusal
- Allergy to local anaesthetic
- Active infection at the site of the block
ANATOMY
The wrist, hand and fingers are supplied by six nerves:
- The median nerve
- The ulnar nerve
- The dorsal branch of the ulnar nerve
- The radial nerve
- The posterior interosseous nerve
- The anterior interosseous nerve
All six originate from the brachial plexus and descend into the forearm to supply the distal structures.
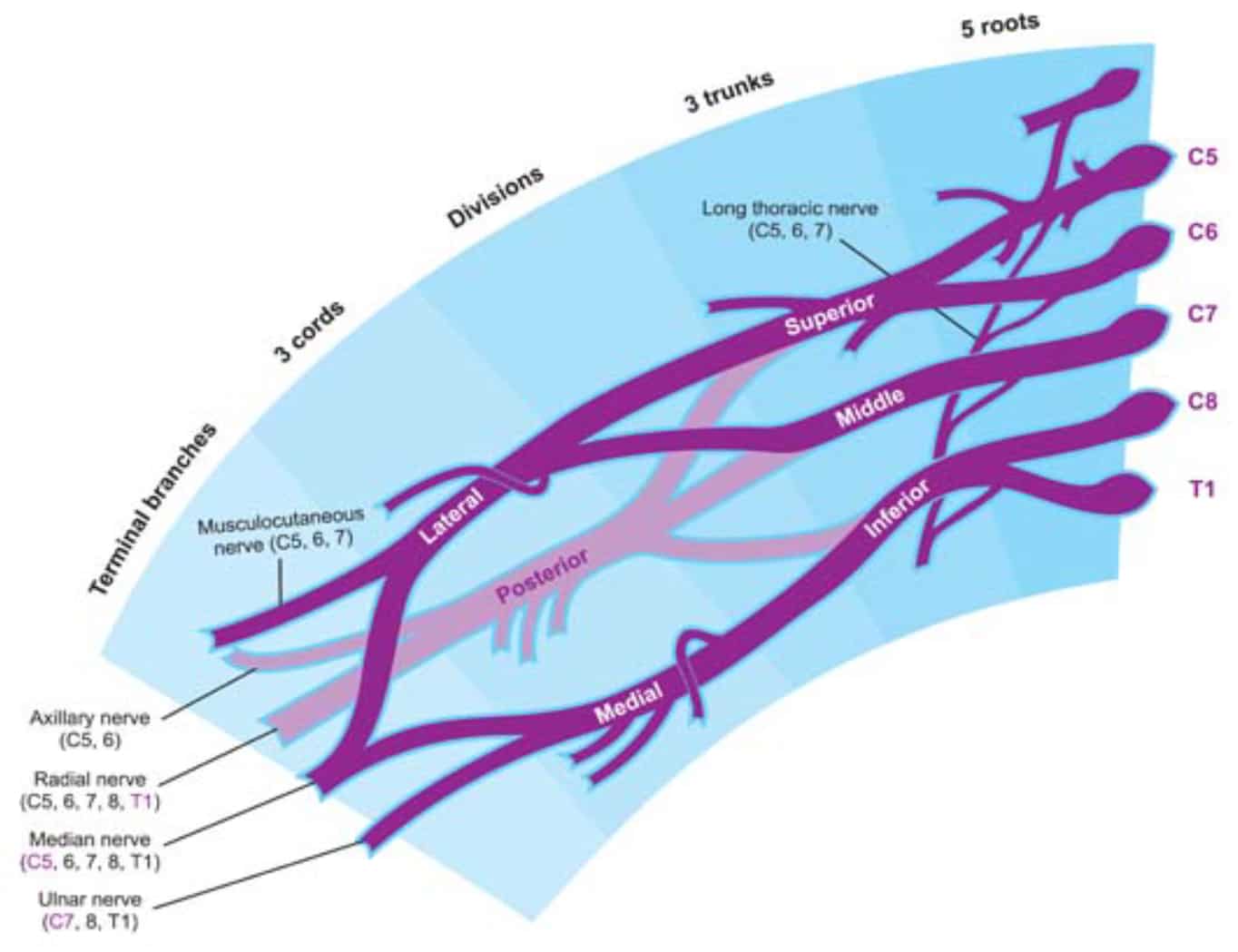
Figure 1: The Brachial Plexus
The Median Nerve
The median nerve arises from the medial and lateral cords of the brachial plexus and takes fibres from nerve roots C5-8, T1 (Figure 1). It has no branches above the elbow but in the forearm supplies the flexor muscles of the forearm (except flexor carpi ulnaris), opponens pollicis, abductor pollicis brevis and the 1st and 2nd lumbricals. Sensory fibres supply the palmar surface of the radial three and a half fingers and their nailbeds. At the level of the wrist, the median nerve traverses the carpal tunnel and terminates as digital and recurrent branches. The digital branches supply the skin of lateral 3½ digits and, usually, the lateral two lumbricals. A corresponding area of the palm is innervated by palmar branches that arise from the median nerve in the distal forearm. The recurrent branch of the median nerve supplies the three thenar muscles. It may be seen that the median nerve must be blocked proximally to the exit of the palmar branches in order to provide complete anaesthesia of the hand (Figures 2 and 3).
The Ulnar Nerve
The terminal branch of the medial cord forms the ulnar nerve, with fibres coming from nerve roots C7-8, T1 (Figure 1). In the forearm, it supplies flexor carpi ulnaris and half of flexor digitorum profundus. In the hand, the deep branch of the ulnar nerve accompanies the deep palmar arch and supplies innervation to the three hypothenar muscles, the medial two lumbricals, all the interossei, and adductor pollicis. Digital branches provide cutaneous sensation for the medial one and a half fingers. The medial palm is supplied by palmar branches that arise from the ulnar nerve in the distal forearm.
The Dorsal Branch of the Ulnar Nerve
The dorsal, medial side of the hand is supplied by the dorsal branch of the ulnar nerve, which arises proximally to the wrist crease. (Figures 2 and 3).
Tip: Although there may be variability of innervation of the ring and middle fingers, the skin on the anterior surface of the index finger and thumb is always supplied by the median nerve and that of the little finger by the ulnar nerve.
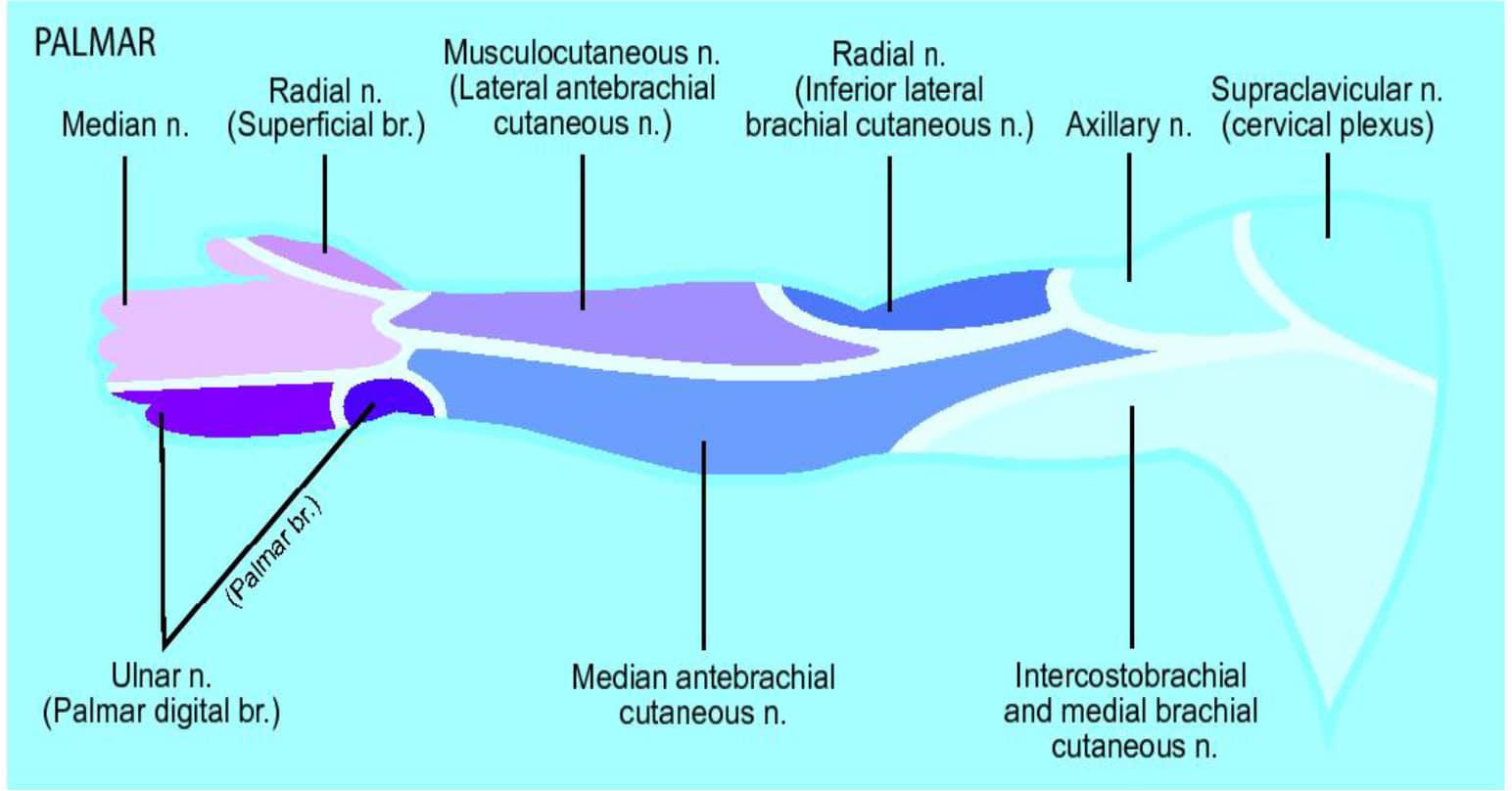
Figure 2: Nerve supply of the arm, palmar surface
The Radial Nerve
The radial nerve is formed from the terminal branch of the posterior cord of the brachial plexus and takes fibres from nerve roots C5-8,T1 (Figure 1). It travels in the posterior compartment of the upper arm and divides at the level of the elbow into the superficial radial nerve (SRN) and the posterior interosseous nerve (see below). The SRN passes distally on the radial side of the forearm with the radial artery and sensory fibres supply the skin of the lateral aspect of the arm, posterior aspect of the forearm and web space between thumb and index finger (Figures 2 and 3). About 7.5cm above the wrist, it leaves the artery, pierces the deep fascia to become superficial and divides into two main branches. The external branch, the smaller of the two, supplies the skin of the radial side and base of the thumb. The internal branch communicates with the posterior branch of the lateral cutaneous nerve. On the back of the hand, it forms an arch with the dorsal cutaneous branch of the ulnar nerve but does not anastamose with it.
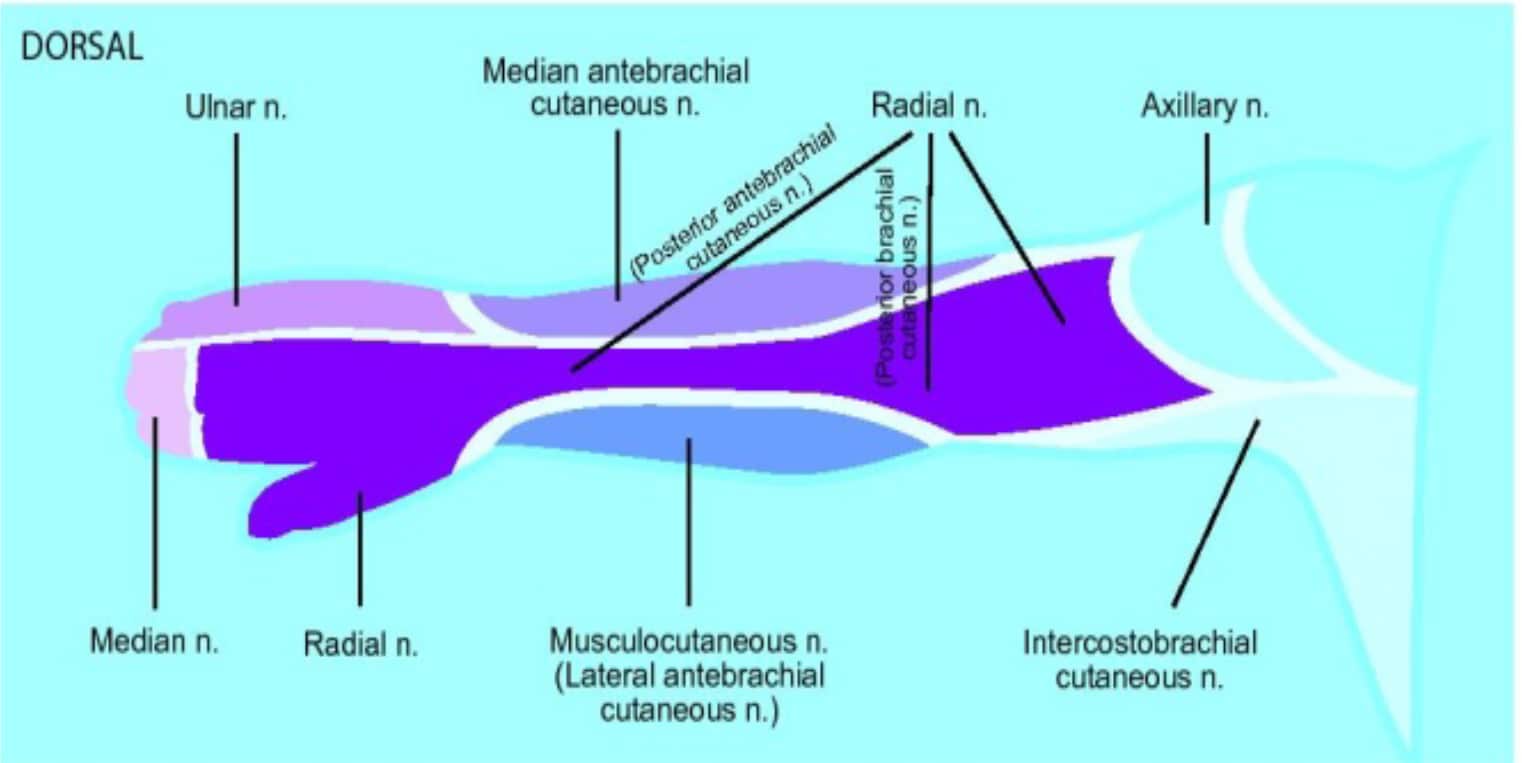
Figure 3: Nerve supply of the arm, dorsal surface
The Posterior Interosseous Nerve
The posterior interosseous nerve (PIN) is the continuation of the deep branch of the radial nerve, taking fibres from nerve roots C7 and C8. It descends on the posterior surface of the interosseous membrane to the back of the wrist giving motor supply to the extensor muscle bellies of the forearm. Although it is predominantly a motor nerve, it also provides important sensory fibres to the ligaments and various articulations of the wrist.
The Anterior Interosseous Nerve
The anterior interosseous nerve (AIN) is a branch of the median nerve that accompanies the anterior interosseous artery along the anterior surface of the interosseous membrane of the forearm, in the interval between the flexor pollicis longus and flexor digitorum profundus, ending in the pronator quadratus muscle and wrist joint. Like the PIN, it is a predominantly motor nerve but contributes important sensory fibres to the wrist joints.
TECHNIQUE
Preparation and Positioning
Fully prepare the equipment and patient, including obtaining informed consent. Also ensure that intravenous access, monitoring and full resuscitation facilities are available. For a more detailed explanation on preparation see ATOTW 134 “Peripheral nerve blocks – Getting started”.
The patient is in the supine position with the arm abducted. Prepare the skin with anti-septic solution.
The Radial Nerve
Landmarks (Figure 4)
The superficial branch of the radial nerve (SRN) runs along the medial aspect of the brachioradialis muscle. It then passes between the tendon of the brachioradialis and radius to pierce the fascia on the dorsal aspect. Just above the styloid process of the radius, it gives digital branches for the dorsal skin of the thumb, index finger, and lateral half of the middle finger. Several of its branches pass superficially over the anatomic “snuff box”.
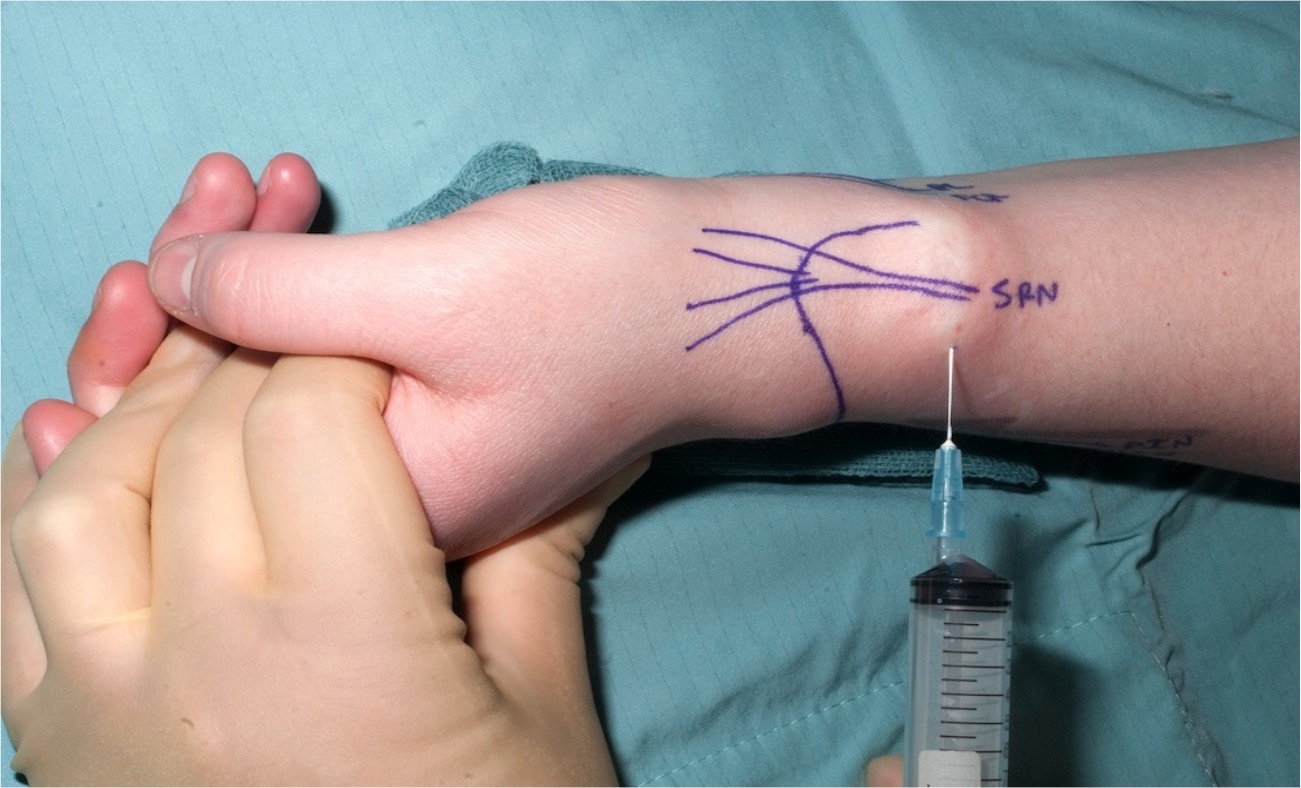
Figure 4: Blocking the superficial branch of the radial nerve
Technique (Figure 4)
The radial nerve is essentially a “field block” and requires a more extensive infiltration because of its less predictable anatomic location and division into multiple, smaller, cutaneous branches. With the wrist held in slight dorsiflexion, local anaesthetic should be injected subcutaneously, 3cm proximal to the radial styloid, aiming medially and towards the radial artery but not piercing it. The infiltration is then extended laterally, using up to5 ml of local anaesthetic.
The Median Nerve
Landmarks (Figure 5)
The median nerve is located between the tendons of the palmaris longus (PL) – present in approximately 85% of the population and the flexor carpi radialis (FCR). The palmaris longus tendon is usually the more prominent of the two; the median nerve passes just deep and lateral to it.
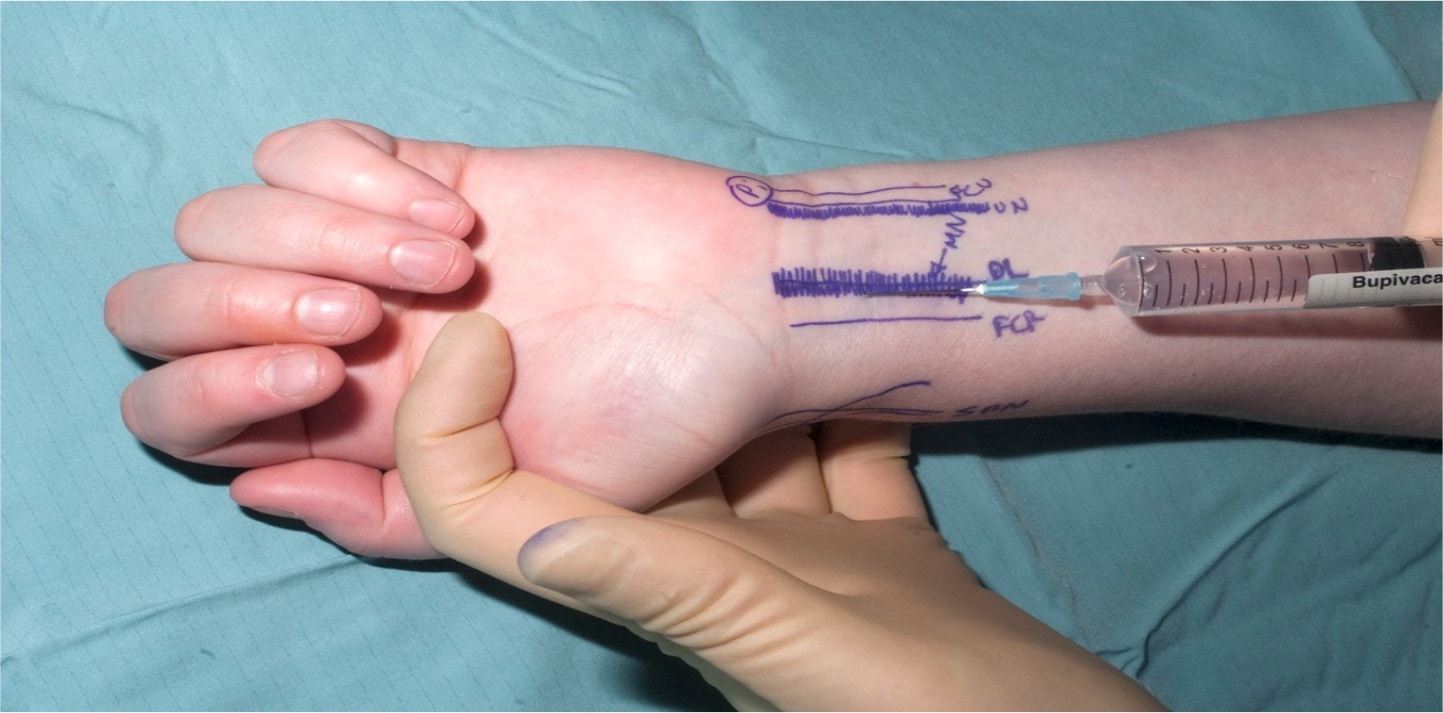
Figure 5: Blocking the median nerve (the needle is inserted between palmaris longus and flexor carpi radialis
Technique (Figure 5)
The median nerve is blocked by inserting the needle 2.5cm proximal to the wrist crease between the tendons of palmaris longus and flexor carpi radialis with the forearm is supinated. The needle is inserted until it pierces the deep fascia (3-5mm). 3 to 5 ml of local anaesthetic is injected. Although the piercing of the deep fascia has been described to result in a fascial “click”, it is more reliable to simply insert the needle 3-5mm as the fascia here is relatively thin and the classical click will not be felt. The median nerve is superficial at this level, proximal to the carpal tunnel and can easily be penetrated by the needle. Any lancinating symptoms into the fingers felt by the awake patient on needle insertion should prompt withdrawal of the needle because this may indicate that the needle is intraneural. Injection should be easy and with relatively low pressure. Pain in the fingers should not be felt by the awake patient during injection.
The Ulnar Nerve
Landmarks (Figure 6)
The ulnar nerve passes between the ulnar artery and tendon of the flexor carpi ulnaris (FCU). The tendon of the flexor carpi ulnaris is superficial to the ulnar nerve, which is the medial to the artery.
The dorsal cutaneous branch of the ulnar nerve (which must be blocked if anaesthesia to the ulnar aspect of the back of the hand is required) curves around the ulnar aspect of the wrist, 1cm distal to the ulnar styloid in the mid-axial plane to reach the skin of the back of the hand.
Technique (Figures 6 and 7) The ulnar nerve is anesthetised by inserting the needle under the tendon of the flexor carpi ulnaris muscle close to its distal attachment just above the styloid process of the ulna. The needle is advanced 5-10 mm to just past the tendon of the flexor carpi ulnaris and 3 to 5 ml of local anaesthetic solution is injected. If blood is aspirated prior to the injection, redirect the needle more superficially and medially as the ulnar artery has been pierced. As with the medial nerve injection, any lancinating symptoms into the fingers felt by the awake patient on needle insertion should prompt redirection.

Figure 6: Blocking the ulnar nerve (the needle is inserted under flexor carpi ulnaris)
A subcutaneous injection of 2-3 ml of local anaesthesia just distal to the ulnar styloid with the forearm pronated is also advisable in blocking the cutaneous branches of the ulnar nerve which often extend to the hypothenar area and the back of the hand.

Figure 7: Blocking cutaneous branches of the ulnar nerve
Interosseous Nerves
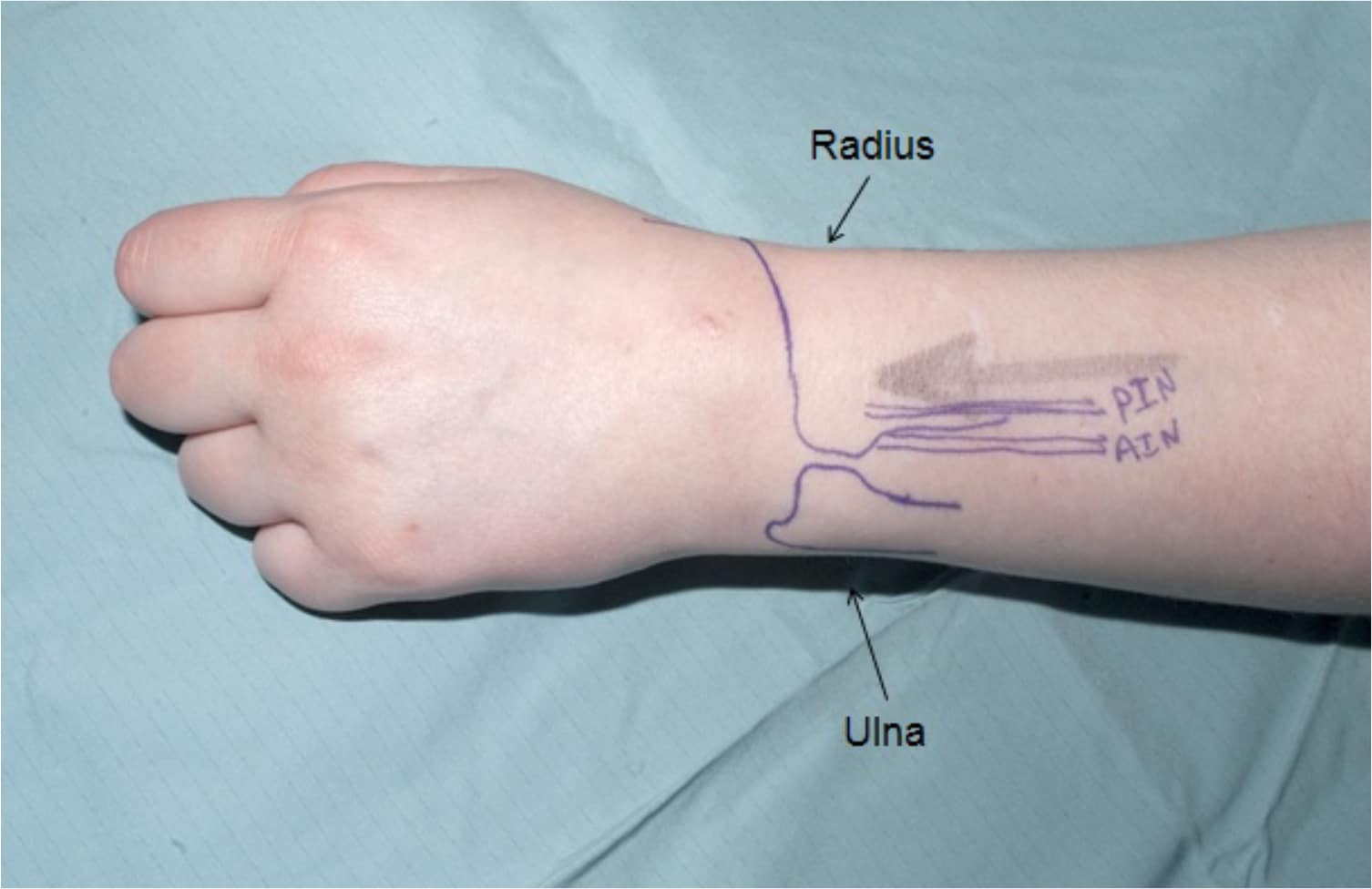
The Posterior Interosseous Nerve (PIN)
Landmarks (Figure 8)
The distal articular branch of the PIN lies alongside Lister’s tubercle at the level of the wrist, before passing proximally between extensor carpi radialis longus and extensor digitorum.
The Anterior Interosseous Nerve (AIN)
Landmarks (Figure 8)
Although the distal articular branch of the AIN is an anterior structure, it is best reached from the posterior aspect of the wrist. Its landmark, therefore, is the radial border of the distal ulnar.
PIN Block
Technique (Figure 9)
With the forearm pronated, the PIN is blocked by an injection of local anaesthetic at the palpable ulnar border of the distal radius, 3 cm proximally to the level of the palpable ulnar head. The needle is inserted until it contacts the radial cortex and the anaesthetic is injected onto the periosteum where the nerve lies. 2ml is adequate.
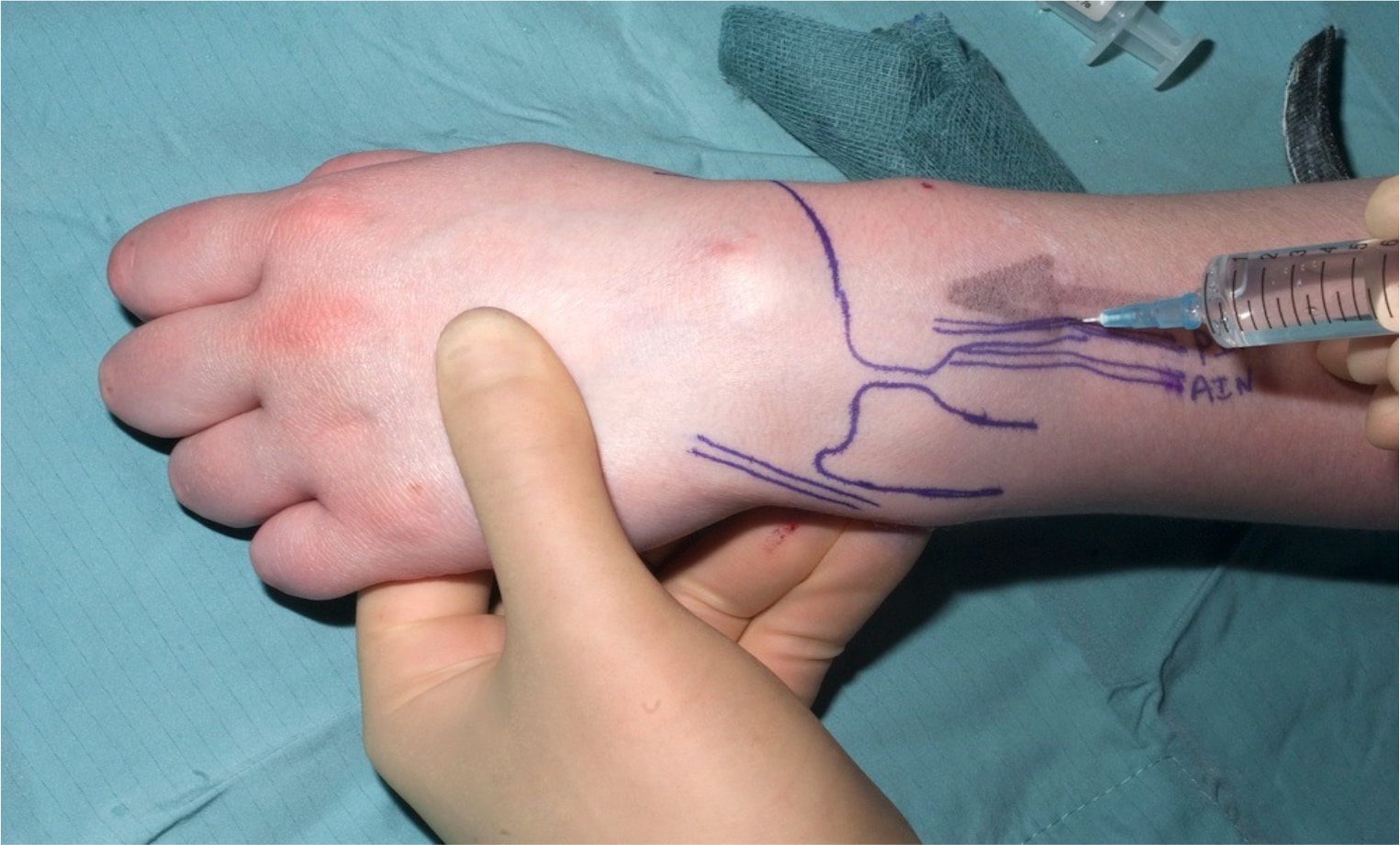
Figure 9: Blocking the PIN
AIN Block
Technique (Figure 10)
Having blocked the PIN, the needle is walked off the ulnar border of the radius and passed between the radius and ulna, through the interosseous membrane, where a “click” is felt. A further 2ml of anaesthetic solution is delivered just anterior to the interosseous membrane where the AIN lies.
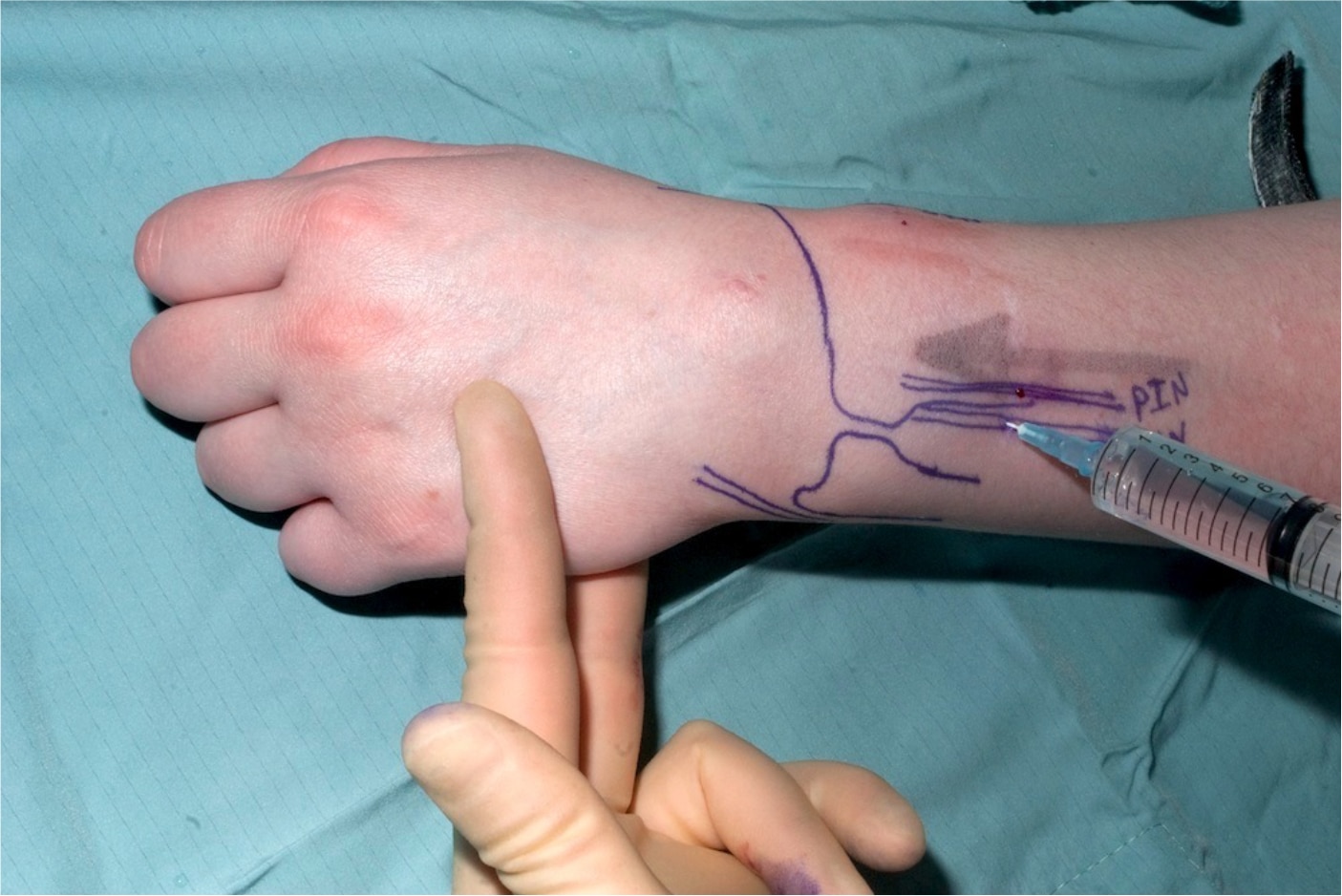
Figure 10: Blocking the AIN
LOCAL ANAESTHETIC
The choice of the type and concentration of local anaesthetic for wrist block depends upon the preferences of the individual operator. Whatever the requirements, the total dose should be well within the therapeutic limit / safe dose because the volumes required are not large. To provide anaesthesia and post-operative analgesia, the authors use 15 ml of a mixture of equal parts of 2% lignocaine and 0.5% levobupivacaine, occasionally increasing this to 20 ml. For post-operative analgesia alone, the authors use up to a total of 15 ml 0.5% levobupivacaine. In order to ensure a consistent “feel” for the injections, the authors also always use a 10 ml syringe and 23G (blue) needle, whatever the volume used.
COMPLICATIONS
- Block failure – in experienced hands the success rate is 98-100%
- Bleeding and haematoma
- Inadvertent vascular injection
- Infection
- Nerve damage – this can result from direct trauma, haematoma or high concentrations of LA and vasopressor. Incidence ranges from 1 in 2,000 to 1 in 50,000
KEY POINTS
- Remember to fully prepare the patient and equipment
- Always aspirate before injecting LA
- Ensure the surgical site is known and all the necessary nerves blocked.
ANSWERS TO QUESTIONS
- Answer d – 6 nerves supply the wrist joint (see text)
- Answer d is true – the anterior interosseous nerve is a branch of the median nerve
- Answer c is false – the median nerve does not have several branches in the upper arm.
WEB LINKS
- The New York School of Regional Anaesthesia – www.nysora.com
- Neuraxiom – www.neuraxiom.com
- RA Education – www.raeducation.com
- Nerveblocks.net – www.nerveblocks.net
FURTHER READING
- Ferreres, A., Foucher G and Suso S, (2002). “Extensive Denervation of the Wrist.” Techniques in Hand & Upper Extremity Surgery 6(1): 36-41.
ACKNOWLEDGEMENTS
- Photographs from personal archive of Mr A. Kocheta. Reproduced with permission.
- Diagrams of the brachial plexus and nerve distribution of the arm, courtesy of Edwina Kelly. Reproduced with permission.



